 I hope that you will find the following posts on what is new and controversial in Medicine, Cancer Prevention, and Nutrition interesting.
I hope that you will find the following posts on what is new and controversial in Medicine, Cancer Prevention, and Nutrition interesting.
If you are confused as to what your target blood pressure should be, you are in good company. Every decade or so the NIH/National Heart, Lung, and Blood Institute (NHLBI) convenes a group of experts to reach a consensus on the desired numbers. The most current national guidelines, known as JNC 8 (Eighth Joint National Committee), were released just last year and recommended a number of changes in target blood pressure recommendations for the systolic (the upper number) and the diastolic (the lower number).
Why the upward change? Part of the answer lies in the changing role of the expert committee. In prior years the experts would pool their personal and research expertise, debate the meaning of the vast literature, iron out their differences, and come up with an updated set of recommended standards.
However, reflecting a pervasive trend in medicine nowadays called “Evidence Based Medicine,” the experience of experts (as well as your doctor) is increasingly minimized. In the Evidence Based Medicine era published studies are king. If they don’t support a point of view beyond a shadow of a doubt, then that point of view is not considered.
In this instance, since the literature to date has not conclusively shown that lower blood pressure is necessarily better and the opinions of the experts were throttled, the committee really had no choice but to set the target goals higher.
So, with that in mind, even though many physicians were uncomfortable with the recommendations, it seemed as if these were to be the new standard for probably another decade until JNC 9 would come along.
A New Standard? – Treat by press release
Last month the NHLBI issued a press release. It said that an ongoing trial that they were conducting known as SPRINT that began in 2013 and which was scheduled for completion in 2018 was stopped early because it showed that treating the upper level of blood pressure (systolic) to a target of 120 seemed better than treating to a less stringent goal of 140. This self-proclaimed breakthrough was quickly picked up by the news media; suddenly it seemed we needed to change our approach to hypertension and once again lower our target goals.
What wasn’t mentioned in the 30-second news flashes was that to get to a systolic blood pressure of 120 would often take up to four medicines, that only 9000 people were in the study, that diabetics were not part of the study, and that the study was yet to be published – let alone reviewed by outsiders; which is an important tenant of evidence based medicine.
Personally I think it was unfortunate that the NHLBI issued a press release on this. The media and the public do not understand that press releases are not the final word. It would have been better for the study to have been published first and critically reviewed by outside experts. For all we know outside experts might ultimately conclude that the study was flawed or stopped too early. So now what should patients and doctors do?
I do suspect that ultimately this newer study, once validated, will again tilt us towards tighter blood pressure goals. However, we have to recognize that medicine is not black and white; there are lots of grays. Arteriosclerosis and its complications are a lifetime in the making, perhaps even starting in the womb; and we may never have definitive answers from short term studies. Treatment decisions about blood pressure need to be individualized as much as possible. For the elderly, in particular, side effects secondary to excessive treatment causing falls, may be their biggest threat.
At the end of the day, guidelines should be recognized for what they are – guidelines. If your health care provider is deciding how to treat you strictly based on the guidelines on their iphone, it might be time to change. A nuanced and individualized discussion with an experienced physician who understands your needs should be your expectation.
Next Post: Cholesterol – How Low Should We Go?
This article first appeared in the November 11 2015 issue of The Greater Olney News
 Learn About Strategies for Healthy Eating and Weight Loss while enjoying a sumptuous meal specially prepared by the Inn at Brookeville Farms Chef Paul just for us! Meet author Rick Weissinger RD,MS, Local Behavioral therapist Andrea Lopes LCSW, and Medical Columnist for the Greater Olney News Dr Ed Taubman
Learn About Strategies for Healthy Eating and Weight Loss while enjoying a sumptuous meal specially prepared by the Inn at Brookeville Farms Chef Paul just for us! Meet author Rick Weissinger RD,MS, Local Behavioral therapist Andrea Lopes LCSW, and Medical Columnist for the Greater Olney News Dr Ed Taubman
Bring a Friend and Save! Seating is limited Click Here To Register
We now think of cancer as a disease of our genes – an accumulation of genetic mutations that may one day show up as a cancerous lump.
Genes are the instruction sets of life; we each start out with over 20,000 pairs of them in each and every one of our cells. As we grow and age, our cells are duplicated hundreds of millions of times, and with each cell division the genetic instruction set is duplicated, as well. Think of asking your secretary to copy by hand 20,000 books containing three billion letters, a hundred million times, and tell her or him that their job is dependent on no mistakes being made.
Part of the miracle of life is that we have evolved an elaborate set of genetic spell checkers that seek out and find genetic misspellings that may develop and fix them. Unfortunately, the system is not perfect; and genetic misspellings in a breast cell, say, can begin accumulating until a cancer develops. Many other factors are being increasingly recognized in the development of cancer, including environmental exposures that increase genetic damage and the role of our immune systems, which can seek out and destroy developing cancers. And there may well be a strong element of randomness, which some prominent researchers refer to simply as “bad luck. Nonetheless, around 5 percent to 10 percent of breast cancers have a strong hereditary component that can be passed on from one generation to the next. In some of these families, the cause has been linked to the genetic spell checkers themselves having genetic misspellings that have been passed down from generation to generation by both men and women over thousands of years. When these “guardians of the genome” are themselves defective, then lifetime cancer risk can rise dramatically. In the mid-1990s researchers separately discovered two different genes that, when misspelled, greatly increased a woman’s risk of developing breast cancer. The first discovered breast cancer-associated gene we now call BRCA1; the second discovered gene is BRCA2.
Recently, genetic testing companies have put together panels of many additional genes to test for breast cancer risk. These panels can sometimes add more confusion than clarity as they often find variations in genetic spelling of unknown significance in lesser-known genes.
Though most patients and physicians think of breast cancer when they hear BRCA, it is the ovarian cancer risk that is potentially more deadly. A woman who has inherited a deleterious BRCA gene has up to a 40 percent lifetime risk of developing ovarian cancer, compared to about a 1 percent to 2 percent risk in the general population.
Unlike breast cancer, ovarian cancer is not detected by self-exam, and screening tests have been repeatedly found to be ineffective. Thus, if a woman is found to have a pathogenic BRCA misspelling, otherwise known as a deleterious mutation, then her ovaries should be removed as soon as child-bearing is completed. Because of the high rate of breast cancer, some women elect to have bilateral mastectomies with reconstruction, while others choose intensive surveillance with MRI screening as a complement to mammography.
The incidence of these cancer-predisposing BRCA genes in the general population is about one in 400 to one in 1,000, with the incidence in the American Jewish population much higher at about one in 40. Given the high incidence in the Jewish population, a strong case can be made to offer BRCA genetic screening to all of Jewish descent. Ovarian cancer at any age, early breast cancer, bilateral breast cancer and male breast cancer should raise hereditary suspicions. If you come from a small family with mostly men, your cancer family history may not be a reliable indicator of your true risk. Before testing, patients should be counseled about the true meaning of not only positive and negative tests but also variants of unknown significance. Also, care needs to be taken to make sure the most appropriate person in the family, the one most likely to be positive, is tested first. A negative test in an individual only has true meaning when there is an identified deleterious mutation in the family.
When someone is battling cancer, hereditary counseling and testing often need to take a back seat. Unfortunately, when the crisis has passed, even at the best cancer centers, we may collectively forget to ask the question as to why the patient got cancer in the first place. Finding a culprit genetic misspelling in a cancer-prone family gives other family members a chance and a choice to be tested to see if they, too, are at very high cancer risk and to take preventative measures. Unfortunately, a recent study showed that only 3 percent of individuals at high risk of an inherited cancer syndrome ever get referred for cancer genetic counseling.
At the end of the day, we can’t do anything about “bad luck,” but we do have control of environmental exposures. Numerous studies have linked being overweight, hormone ingestion and alcohol consumption, even in small doses, to increased breast cancer risk. So if you are worried about breast cancer, try to eat less meat, consume more fruits and vegetables, minimize your alcohol consumption, start exercising and begin shedding pounds. If you family history is of concern, ask your doctor to refer you to a cancer genetic specialist.
Dr. Edward Taubman has been practicing primary care medicine in Olney since 1979. He is a graduate of the City of Hope Intensive Cancer Genetics Program and a member of the National Society of Genetic Counselors andthe Fisher Center for Hereditary Cancer and Clinical Genomics Research.
This article first appeared in the Greater Olney News on October 28, 2015
 It’s that time again: Kids back in school, weather getting a bit cooler, and folks thinking about flu vaccinations. The CDC recommends that everyone six months and older be vaccinated.
It’s that time again: Kids back in school, weather getting a bit cooler, and folks thinking about flu vaccinations. The CDC recommends that everyone six months and older be vaccinated.
Flu strains change from year to year, so there is always a tricky dance between the flu strains that are out there in other parts of the world, our ability to predict which ones will predominate in the northern hemisphere this winter, and the manufacturers producing the right amount of vaccine. This year flu vaccines are in good supply. However, the protection requires one to be vaccinated!
Flu vaccines now come in different “flavors” – some are higher dose and intended for seniors, some contain three strains (trivalent) and some four strains (quadravalent). With the exception of the nasal version which is offered to children, none of them contain a live virus; so contrary to popular lore, they are incapable of giving one the flu.
The senior or high dose flu vaccine is entering its fifth year of widespread availability. Knowing that those over 65 don’t always get the protection expected from flu shots, this version contains four times the amount of “antigen” which is what stimulates the immune system to gear up for a possible encounter with a flu virus. The senior version only comes in a trivalent form and is preservative free.
For adults younger than 65, we have our supply of standard dose quadravalent vaccine. The quadravalent vaccine helps to protect against four strains of flu.
We recommend getting your vaccine at the time of a regularly scheduled appointment such as your 3 month diabetes checkup or physical. Others are welcome to walk in during regular office hours. We are not anticipating any shortages of vaccine this year. We spend over 60,000 dollars a year stockpiling vaccines for our patients. Please keep that in mind before you roll up your sleeve at the supermarket. Getting your vaccines here ensures that we have an accurate record of vaccines given to you and remember – if you don’t feel well will the pharmacist be there to take care of you?
Dr. Ed Taubman Olney, MD 301-774-5400
Know someone who is looking for a great primary care practice? We are accepting new patients.
 Saturday mornings Kevin Maselka continues his immensely popular weekly fitness sessions held in collaboration with Integrative Weight Loss Solutions.
Saturday mornings Kevin Maselka continues his immensely popular weekly fitness sessions held in collaboration with Integrative Weight Loss Solutions.
Since 1985, Kevin has been the preferred fitness trainer to exercise newcomers, fitness enthusiasts, Olympic and professional sports athletes, and an impressive list of Washington’s power elite.
Kevin is owner and head trainer at Elite Physique, one of the nation’s oldest and most sought-after fitness firms. Go to olneyweightloss.com to register for the next session and join us.
Thanks to all who attended our own first Olney Health Fair last weekend and special thanks to Barry Schwartz of B.J. Pumpernickel’s who provided healthy food and showed off his weight loss of over sixty pounds through our program. Come Visit Dr. Taubman and Integerative Weight Loss Solutions this Saturday September 19 between noon and 5:00 at the Roots Clarksville Grand-Re Opening and take part in the celebration, fun, free stuff, and sales!
If you remember Peter, Paul, and Mary this is a must listen!
Are You Up To Date?
Routine colonoscopy screening starts at age 50 (or ten years before earliest case of colon cancer in the family)
Followup studies every 2-5 years depending on number of polyps found or colon cancer in the family – Every ten years for everyone else.
Course description: Breast cancer is the second most common cancer in women, and 12% of women will develop this disease. Women tend to believe in a genetic cause for breast cancer, yet only 5%-10% are caused by inherited gene mutations. Several known risk factors for breast cancer exist, and these are influenced significantly by factors under a woman’s control. Unfortunately, women receive practically no sound advice on how to reduce their risk, leaving them no means for preventing this disease. This lecture will bring women up to speed on what the risks for breast cancer are and how to significantly improve their chances for preventing this common cancer. A portion of the proceeds will be donated to the American Institute for Cancer Research, a Washington D.C.- based cancer research and education organization.
Speaker Information:Rick Weissinger, M.S., R.D. spent several years reviewing the scientific evidence linking cancer growth to diet and lifestyle, and interviewed cancer researchers
All attendees will receive a copy of Rick’s book (What the Experts Say About Food and Cancer).
Seating is limited and requires prior registration:
For more information and to get on our waiting list for Rick’s next talk send an e-mail to olneymywellness@olneymedical.com
Notice re upcoming course offered at Montgomery College  This course will address the major components of retiree health care: Medicare, Medicare Advantage Plans, and Long-Term Care.
This course will address the major components of retiree health care: Medicare, Medicare Advantage Plans, and Long-Term Care.
Health care costs typically rise at twice the inflation rate, so the course will also address ways to fund this expense through tax-advantaged plans. You will determine the cost of supplemental coverage, evaluate your ability to pay for health care not covered by federal or state programs, and be able to project your health care expenses.
The target audience for this course is those who are newly retired and those who plan to retire within 10 years.
Tuition waiver applies; seniors pay fee only.
Course: LLI699 5 Hours $60 + $62 fee = $122; Non-Md. residents add $120
Rockville Campus CRN#: 35830
2 Sessions 3/30-4/1 M,W 6:30-9 PM
Registration 240-567-5188
Kindly supplied by Richard Beall

I have tried a lot of diets in my life and can honestly say that this program has been the easiest and most successful. I have lost 22 lbs in 7 weeks and the program has changed my life. The combination of a medical doctor, psychologist, nutritionist, and yoga expert has been a total approach to weight loss. I have yoyo dieted my entire life and had all but given up on my goal of weight loss. I had tried so many times and failed. I was so overweight and was unable to do all the things that I wanted to do. For the first time in my life, I feel like I know how to eat and deal better with emotional eating. I know that I have a ways to go to reach my goal, but I feel confident that this program will get me there.
Debbie Butler, Olney, MD
I sincerely appreciate your help these past 10 weeks. I have learned a lot. I also thank Dr. Taubman for providing such a program. You have equipped me with the tools necessary to continue on this life journey to better nutrition and weight management.
Marilyn Jordan, Olney, MD
I had weight loss surgery and lost over a hundred pounds; Unfortunately I then gradually regained most of it. This is the best and easiest diet I have ever been on. I have lost almost fifty pounds in the past four months while eating normal foods. I feel so much better! Thx so much to Doctor Taubman, Rick, Andrea, and the whole Integrative Weight Loss Team.
Barry (B.J. Pumpernickle’s) Schwartz, Olney, MD
Thank you for the Time and effort you all have put in to make a miracle happen in my life. While over 20 pounds in 7 weeks may not sound a lot to some, To me, who has never lost weight on a diet, this was a life changing event. Thanks for the help with cooking, yoga and mental discipline.
Shiela Hanson, Cloverly, MD
They are vertically integrated to help me take charge of my body, mind and diet – health and wellness – (MD, nutritionist and psychotherapist/counselor). I’ve had terrific success, lost over 60 lbs. in about eight months and I’m given tools and mental, physical training (and even shopping/menu planning) to change my eating/diet and health lifestyle and most importantly, the ability to sustain those changes going forward. These sessions are conducted in a highly collaborative and supporting environment; an opportunity to learn new methods and share with other my very positive experience and benefit from everyone’s “lessons learned”. I’d highly recommend the program and each medical and health professional.
Joe Briglia, Gaithersburg, MD
I was exercising all the time but wasn’t feeling well and couldn’t lose weight. I saw Dr. Taubman asking to adjust my medicines but he said the problem was the kinds of foods I was eating. I was skeptical but needed to do something so I joined the Integrative weight loss program. Dr Taubman was right! I have lost almost twenty pounds and feel so much better. Just the other day my teenage daughter said “Mom, what are you doing – you look great” I highly recommend this program.
Marjory Haddix, Brookeville, MD
 Our open house has come and gone! Attendees heard from former participants Barry Schwartz, Joe Briglia and Marjory Haddix who have lost a total of 150 pounds! It is not too late to join but only a few spots remain for our next ten week session which starts on February 23: To learn more click here. Let us help you to be a happier and healthier you!
Our open house has come and gone! Attendees heard from former participants Barry Schwartz, Joe Briglia and Marjory Haddix who have lost a total of 150 pounds! It is not too late to join but only a few spots remain for our next ten week session which starts on February 23: To learn more click here. Let us help you to be a happier and healthier you!
Did you know that diet directly correlates with your mental health? If you or someone you know suffers from depression, the benefits of a diet makeover are endless! Dr. Taubman, primary care physician at Olney Medical in Olney, Maryland, invites you to join this cutting edge seminar on the latest evidence on the connections between nutrition and mental health.
Presenter: Rick Weissinger, M.S., R.D.
When: Wednesday, January 14, 2015 at 7 pm
Where: Olney Counseling Center
3430 N. High Street
Olney, Maryland 20832
Refreshments and light fare will be served. Seating is limited. Please reserve your seat by clicking here or calling 301-570-7500. Thank you!
During this lecture, you can expect to learn more about:
 Your presenter for the evening will be Rick Weissinger, M.S., R.D. Rick is a registered licensed nutritionist in private practice in Olney, MD and Alexandria, VA. Rick is the author of “What the Experts Say About Food and Cancer” and the co-author of two editions of “Nutrition Guide for Clinicians,” a 900-page handbook for medical students detailing roles for nutrition and lifestyle treatments for most common, chronic health problems. He is currently co-director and founder of Olney Integrative Weight Solutions, along with psychotherapist Andrea Lopes, LCSW-C and Washingtonian “Top Doc” Edward Taubman, M.D.
Your presenter for the evening will be Rick Weissinger, M.S., R.D. Rick is a registered licensed nutritionist in private practice in Olney, MD and Alexandria, VA. Rick is the author of “What the Experts Say About Food and Cancer” and the co-author of two editions of “Nutrition Guide for Clinicians,” a 900-page handbook for medical students detailing roles for nutrition and lifestyle treatments for most common, chronic health problems. He is currently co-director and founder of Olney Integrative Weight Solutions, along with psychotherapist Andrea Lopes, LCSW-C and Washingtonian “Top Doc” Edward Taubman, M.D.
Unable to make the seminar? Don’t worry! You can make an appointment to meet with our nutrition or Dr. Taubman any day of the week. Let us help you re-learn how to eat! Our team of experts will teach you exactly what you need to eat to develop a healthy lifestyle. Contact us online or call 301-774-5400 for more information.
 This coming year will bring many government mandated changes to the practice of medicine. More and more of your health record will need to be transmitted electronically to databases so that it can be analyzed and shared. Effective January 1 Medicare will be lowering reimbursements to practices that do not successfully upgrade to and use “Meaningful Use Version 2” and PQRS (Physician Quality Reporting System). Plus the coding system itself will also be upgraded. Presently there are over 13,000 codes available to assign to your reason for seeing the doctor. Apparently that is not enough so medical staffs in offices and hospitals around the country will need to be retrained to pick from over 68,000 codes. Abdominal pain will no longer be good enough – specifying right sided vs left sided will be necessary.
This coming year will bring many government mandated changes to the practice of medicine. More and more of your health record will need to be transmitted electronically to databases so that it can be analyzed and shared. Effective January 1 Medicare will be lowering reimbursements to practices that do not successfully upgrade to and use “Meaningful Use Version 2” and PQRS (Physician Quality Reporting System). Plus the coding system itself will also be upgraded. Presently there are over 13,000 codes available to assign to your reason for seeing the doctor. Apparently that is not enough so medical staffs in offices and hospitals around the country will need to be retrained to pick from over 68,000 codes. Abdominal pain will no longer be good enough – specifying right sided vs left sided will be necessary.
Now the government line on this is that more specific electronic reporting will make for better accountability by the medical profession and lead to a healthier population while lowering costs. Sounds like a good idea until you understand how much of the physician and staff time will be spent in these endeavors. Personally I feel that better medical care is delivered when your doctor can be looking at you rather than at a computer screen and spending time actually poking around your abdomen that worrying what code to put down; and to get on the phone with a consultant rather than sending an imperfect electronic summary.
So make believe you are my assistant and we need to learn the newer requirements that come with each and every visit. Please accompany me as we listen to a training video explaining all the steps involved by Clicking Here Remember that this is just one small part of what we will be required to be doing on top of all the other things we normally do to make your visits pleasant and productive.
After viewing the video let us know if you find this “Meaningful” or “Useful” to the delivery of your health care! And remember it only gets more convoluted – Meaningful Use Version 3 is just two years down the road! In a future blog I will take a closer look at the PQRS measures that Medicare uses to monitor “Quality” and the accompanying documentation burden on health care providers.
Thanks for reading – Please share with others – Links Below! Click Here to start receiving my health blog summary via email. Until next time…. Dr Ed Taubman, Primary Care Doctor, Olney MD 301-774-5400 Know someone who is looking for a great primary care practice? We are now accepting new patients!
 Despite that eye catching photo there really is no drama involved in getting your blood work done at Olney Medical. For your convenience our skilled and pleasant phlebotomist Brittany is present every day that we are open from 8:00 to Noon. No appointment is necessary.
Despite that eye catching photo there really is no drama involved in getting your blood work done at Olney Medical. For your convenience our skilled and pleasant phlebotomist Brittany is present every day that we are open from 8:00 to Noon. No appointment is necessary.
We are now sending lab specimens collected in our office to Everest Medical Lab, Boston Heart Lab and Singulex Lab. We may use one or all of these labs for your blood work. We have chosen these labs for their high level of service and their cutting edge technologies, which help us to catch diabetes and heart disease at its earliest stages, and importantly their affordability for our patients.
These advanced tests do require more time to come back and you may also note that an extra tube or two of blood will be drawn than you may be used to. If you are having your bloodwork for an upcoming physical please try and have your blood drawn at least two weeks in advance so that we will have the results ready for your visit. If your blood sugar or cholesterol is being tested try and not eat for 8 hours – but stay well hydrated by drinking water or black coffee.
Since Everest, Boston Heart, and Singulex labs are not in network for some insurance plans, you may receive an Explanation of Benefits (or EOB) from your insurance company showing a large sum that was not covered by your insurance company for your lab work. You can ignore this sum because Everest, Boston Heart and Singulex normally do not send out bills to our patients. If you see the word “pathology” in your insurance company EOB do not be concerned; some insurance company computers such as Carefirst routinely code blood tests as “pathology”. AGAIN, YOU SHOULD NOT RECEIVE BILLS FROM THESE LABS FOR YOUR LAB WORK. Your only obligation to prevent being billed is to forward any checks you might receive from your insurance company to the appropriate lab. In such cases kindly endorse the check and mail it with a copy of Explanation of Benefits to the appropriate lab:
Everest Medical Lab 99-107 Glendale Ave, Edison, NJ 08817 Phone 732-777-9222
Boston Heart Boston Heart Diagnostics P.O.Box 842856 Boston, MA 02284-2856 Phone 508-877-8711 x337
Singulex, 1701 Harbor Bay Parkway #200, Alameda, Ca 94501 Phone 510-995-4763
This is a win – win for everyone involved. You get the latest technology tests from cutting edge labs with no financial responsibility to you (while helping to satisfy any deductibles you may have). Plus, these arrangements allow us to provide on-site phlebotomy so you don’t need to go downstairs and wait in a crowded drawing station.
We Hope this answers any questions you may have. Please contact us via e-mail Rebecca@olneymedical.com or phone 301-774-5400 if you have further questions.
 Why do some people seem to retain their mental faculties far into their advanced years while others become more forgetful sooner? And is there anything that has been proven to prevent the loss of memory and cognitive function later in life? These issues were recently highlighted in an edition of Science magazine.
Why do some people seem to retain their mental faculties far into their advanced years while others become more forgetful sooner? And is there anything that has been proven to prevent the loss of memory and cognitive function later in life? These issues were recently highlighted in an edition of Science magazine.
Understanding the normal process of aging is a first step in trying to explain what happens later in life. Researchers are finding intriguing clues to the normal process of brain aging by analyzing data from the so-called Scottish Mental Studies. In 1947 70,000 Scottish children, all eleven years old, were administered an IQ test that lasted 45 minutes. Starting in 2004 about 1000 survivors from the original group were contacted and asked to retake the same IQ test to see how they had fared. They were also asked to provide DNA samples, share diaries of their lifestyles including food and alcohol, and have MRI scans of their brains. The results have generated more than 250 scientific papers.
So far the results have shown that the best predictor of one’s IQ later in life is ….drum-roll……one’s IQ earlier in life; which also correlates with the thickness of the outer surface of the brain as measured by MRI later in life. These studies suggest that about half the differences among people’s mental abilities seen later in life can be attributed to how intelligent they were as children. Perhaps as much as a quarter of the differences may be attributed to still be defined genetic causes.
Clearly the causes of memory decline and even improvements seen in some people but not others over time remain to be determined; learning how the brain functions both in health and disease will take many, many years. However, the Scottish study gives researchers a starting point to test new theories and perhaps one day come up with interventions. Having and maintaining a healthy and inquisitive mind in childhood may ultimately prove to be the best protector of brain function in adulthood.
Thanks for reading – Please share with others – Links Below! Click Here to start receiving my weekly health blog post via email. Until next week…. Dr Ed Taubman, Primary Care Doctor, Olney MD 301-774-5400
Know someone who is looking for a great primary care practice? We are now accepting new patients!
There has been a lot of hype about the Paleo Diet and its health benefits. The basis of the diet is to eat only things you can hunt and gather—like a caveman. The virtues of “eating like a caveman” are praised on sites such as Living Super Human. I asked our nutritionist, Rick Weissinger, author of “What the Experts Say About Food and Cancer,” to comment on the virtues of a diet that promotes meat and egg yolks while shunning legumes (beans, lentils, peas, and peanuts, etc.). His comments follow:
Recently, Dr. Taubman alerted me to posts regarding the Paleo diet that he thought I should comment on. Below are some of the statements made by Paleo enthusiasts about beans and other legumes along with my views on the matter. If I don’t sound convincing enough, please read Dr. McDougall’s post on The Paleo Diet Is Uncivilized.
“Most legumes are extremely toxic in their raw state.”
Why is this a problem? No one eats these foods raw. Why don’t you try eating hamburger and chicken raw, and compare the toxicity of these with legumes? You can write about it while you’re recuperating in the hospital!
“Phytates found in legumes, specifically phytic acid, have been shown to block the mineral absorption of calcium, magnesium, iron, and zinc.”
Phytic acid, also known as phytate or as inositol hexaphosphate (IP6) is also an incredibly potent anti-cancer phytochemical, as I discussed in my book. The science is actually crystal clear that the reduced absorption of IP6 that occurs from eating legumes and whole grains does not pose a risk for making people deficient in these minerals.
Want to know about your heredity risk of cancer? Dr. Taubman offers Cancer Genetic Counseling.
“Phytates have also been shown to inhibit important enzymes involved in digestion, including pepsin and amylase.”
These properties actually have the potential to help with weight loss; they shouldn’t be avoided, they should be increased in our diets.
“Soy leads to an increased risk of bladder cancer.”
This was found in ONE study. All the other evidence has shown a LOWER risk of bladder cancer with higher soy intake, consistent with the effect of soy on several other common cancers.
“Soy fed infants have more reproductive and asthma issues as adults.”
On the contrary, a 2001 article in the Journal of the American Medical Association concluded that “Exposure to soy formula does not appear to lead to different general health or reproductive outcomes than exposure to cow milk formula.”
“Increased consumption of soy-based tofu led to lower cognitive function later in life and a greater incidence of Alzheimers.”
On the contrary, several studies have demonstrated that soy isoflavone (SIF) supplementation can improve aspects of cognitive function, and the phytoestrogens in soy have been shown to reduce Alzheimer’s Disease (AD) related pathology.
“The Paleo diet shuns processed foods and Paleo followers are cooking more at home.”
Any diet should get people to eat at home more. This is not justification for eating meat, eggs, and cheese three times or more each day; animal meats and products have been associated with higher inflammation in the body. Inflammation is linked to many chronic ailments including heart disease, cancer, diabetes, and arthritis.
“Egg yolks are good for you and don’t really raise your cholesterol.”
Sounds like a great topic for next week’s blog!!
If you are interested in learning more about nutrition, weight loss solutions, and the steps you need to take to get healthy, schedule an appointment with Dr. Taubman and our certified nutritionist!
If you are interested in starting a new diet, consult your physician first. Fad diets can often be dangerous. It is important to eat a well-balanced diet with whole foods that offer the right nutrients for your body. To learn more about dieting and starting a healthy diet regimen, contact Dr. Taubman at Olney Medical to schedule an appointment at our office in Olney, Maryland!
 One of my favorite recent articles is a review by Dr Christopher Labos in Medscape describing why what we read in the medical literature is not always correct. If it is reported as published in the New England Journal of Medicine we tend to believe it true. Unfortunately, all studies are subject to errors ranging from flawed assumptions to just plain chance. Ultimately for a study to be accurate it should withstand the test of time and be replicated – which is really the scientific method. However not all studies are replicated. Lobos cites a review of 45 studies in major medical journals; 24% were never replicated, 16% were contradicted by further studies, and in 16% the effect reported turned out to be smaller than originally reported. Some of the associations reported in the past which made headlines and which have turned out to be false include: Coffee consumption increases pancreatic cancer risk, cell phones cause brain tumors, and estrogen replacement prevents heart disease. Something to think about when you read about the next breakthrough.
One of my favorite recent articles is a review by Dr Christopher Labos in Medscape describing why what we read in the medical literature is not always correct. If it is reported as published in the New England Journal of Medicine we tend to believe it true. Unfortunately, all studies are subject to errors ranging from flawed assumptions to just plain chance. Ultimately for a study to be accurate it should withstand the test of time and be replicated – which is really the scientific method. However not all studies are replicated. Lobos cites a review of 45 studies in major medical journals; 24% were never replicated, 16% were contradicted by further studies, and in 16% the effect reported turned out to be smaller than originally reported. Some of the associations reported in the past which made headlines and which have turned out to be false include: Coffee consumption increases pancreatic cancer risk, cell phones cause brain tumors, and estrogen replacement prevents heart disease. Something to think about when you read about the next breakthrough.
Until next week. Dr Ed Taubman, Primary Care Doctor, Olney MD 301-774-5400
Like what you are reading? Please share with others!
Know someone who is looking for a great primary care practice? We are now accepting new patients!
Click Here to start receiving my weekly health blog post via email – It’s Free!
 This week, rather than delving in depth on a specific topic I thought I would get off my soapbox and summarize some recent literature that is of interest to me as a physician and which may perhaps have impact on health care in the not too distant future. Let me know what you think of this format!
This week, rather than delving in depth on a specific topic I thought I would get off my soapbox and summarize some recent literature that is of interest to me as a physician and which may perhaps have impact on health care in the not too distant future. Let me know what you think of this format!
-A number of articles and an editorial in the New England Journal of Medicine document that even though the media is focused on new and experimental treatments for Ebola that many lives can, and are being saved, with the use of intravenous fluids, attention to oxygen needs, and treatment of secondary infections. Though such treatments are commonplace in intensive care units such as those in our own community, they are lacking in Africa – which contributes to the high death rate there. In essence Ebola is a serious viral infection which can be treated with existing known management strategies.
-Previously I have touched on the childhood obesity epidemic. So how do we get adolescents, for instance, to cut back on the sodas they are drinking? In a study done by the Johns Hopkins Bloomberg School of Public Health adolescents going to the store were shown how many calories were in the beverages they were consuming vs how many miles they would have to walk to work off a single soda. The authors reported that “adolescents who were given caloric information associated with a sugar-sweetened beverage in a format they could relate to” ie how many miles they would have to walk to work off a single soda were more likely to purchase a smaller sized soft drink, choose a diet beverage, or forgo the beverage altogether. Makes sense to me. Seriously, maybe we should do the same thing on food labels in general.
-So, you’re a drug company and want to test to see if your new drug is better than a placebo (dummy or sugar pill). To get FDA approval you need to spend tens or even hundreds millions of dollars doing trials to prove your drugs are safe and effective. Sounds straight forward; but in actuality many people in drug trials are just like everyday patients – they often don’t take their medicines as directed – which means the researchers doing the study may get ambiguous results or need to enroll many more patients to find true differences among different treatments; doing so makes the trials that much expensive to do which ultimately drives up the cost of the new medicines.
As reported in Science some strategies being discussed to deal with this include putting microchips on pill bottles to show how often the bottles have been opened and even inserting microchips into the pills themselves that can radio to monitoring devices that they have actually been ingested! And finally, researchers have discovered what may be genetic traits that make some people inherently more predisposed to respond to dummy pills or just want to please; in drug trials they may be more prone to report benefits and not report adverse effects. If too many of those people are in drug trials they could influence the results in a way that makes it hard to tell if a drug was better than a dummy pill; in the future genetically testing for such traits to limit the number of such people in drug studies might one day increase the reliability of drug studies, reduce the number needed to find a benefit, and ultimately reduce the cost of bringing new treatments to market.
Until next week. Dr Ed Taubman, Primary Care, Olney MD 301-774-5400
Like what you are reading? Please share with others!
 Just the other day, I had a case where an elderly woman was in a lot of pain, so I called in prescriptions to the local grocery store pharmacist to help alleviate the pain and make her more comfortable. The next day the family called to say she was on the way to the emergency room because the pain had gotten worse. I asked how many of the pain pills she had taken and was told none—the prescription had not yet been filled by the pharmacy.
Just the other day, I had a case where an elderly woman was in a lot of pain, so I called in prescriptions to the local grocery store pharmacist to help alleviate the pain and make her more comfortable. The next day the family called to say she was on the way to the emergency room because the pain had gotten worse. I asked how many of the pain pills she had taken and was told none—the prescription had not yet been filled by the pharmacy.
Concerned about this woman’s prescription I again called the pharmacy. I asked the grocery store pharmacist why it took a day to fill a prescription that I had personally called in, and he told me that they were way behind in processing prescriptions because they were so busy giving flu shots!
Pharmacists too busy giving shots to fill prescriptions? So here I am, back on my soap box to complain about the corporatization of health care at all levels and the accompanying trivialization of the role of primary care in our society.
In primary care circles, there is increasing talk of the demise of primary care medicine; for this and a multitude of reasons. In my one-person doctor office, for instance, we outlay over 60 thousand dollars a year to stockpile immunizations and injectibles; with a large chunk of that going to seasonal flu shots. Every time a patient goes to the grocery store or pharmacy to get a flu shot, a primary care practice somewhere has to struggle that much more. Every time a patient goes to a walk-in clinic for a sore throat or relatively minor illness, it means that a primary care practice has fewer ways to offset the time spent managing more complicated patients, for which reimbursements are inherently low. And so it goes on and on.
It has become more and more acceptable for patients to get their flu shots at the grocery store or pharmacy lured by discounts at the checkout counter, or to go to the walk-in clinic for a minor illness, or to the emergency room for something a primary care doctor could easily diagnose and treat. No longer is there a caring and knowledgeable primary care physician and staff looking at the big picture. The patient becomes his own primary care provider. After consulting the internet, said patient refers himself to more and more specialists who, not knowing the patient, order more and more tests. People then wake up one day and wonder how medicine became so costly and fragmented and wonder why it’s so hard to find a good primary care practice.
The answer to that question starts with that grocery store flu shot.
Until next week this is Dr. Ed Taubman Primary Care, Olney MD, where we still give vaccines, draw our own blood, and give people the personalized care they deserve. Call today to book your appointment with the top primary care doctor practice in town, at 301-774-5400; where friendly and helpful people are ready to serve you and the doctor actually picks up the phone to coordinate your care with your other health care providers.
Like What you are reading? Click Here to start receiving my weekly health blogs sent to your email – It’s Free!
 The recent case of a Liberian with Ebola virus not being recognized by a Dallas emergency room provides a reason for me to get on my soap box and complain about the transformation of American medicine into a checklist mentality. While I understand that checklists can play important roles in certain industries – the classic case being pilots making sure flaps are up before takeoff and nurses in operating rooms making sure all instruments are accounted for after surgery – a checklist mentality has now permeated all aspects of medicine. The problem is there are now so many checklists to be completed that health care workers are too close to the checklist trees; and sometimes miss the big picture. Once checklist A has been completed, then it’s on to checklist B and so it goes, on and on – all in the name of good care. The problem is that medicine has a lot of subtleties; it’s not just black and white but lots of greys. Good clinical judgment cannot be captured by a checklist and good medical care requires great communication. This means people need to talk to each other – which is difficult when one is glued to a computer filling out checklists. Medicine is an art as much as a science; that’s why to become a doctor takes over a decade. There aren’t enough checklists in the world to ensure good medical care.
The recent case of a Liberian with Ebola virus not being recognized by a Dallas emergency room provides a reason for me to get on my soap box and complain about the transformation of American medicine into a checklist mentality. While I understand that checklists can play important roles in certain industries – the classic case being pilots making sure flaps are up before takeoff and nurses in operating rooms making sure all instruments are accounted for after surgery – a checklist mentality has now permeated all aspects of medicine. The problem is there are now so many checklists to be completed that health care workers are too close to the checklist trees; and sometimes miss the big picture. Once checklist A has been completed, then it’s on to checklist B and so it goes, on and on – all in the name of good care. The problem is that medicine has a lot of subtleties; it’s not just black and white but lots of greys. Good clinical judgment cannot be captured by a checklist and good medical care requires great communication. This means people need to talk to each other – which is difficult when one is glued to a computer filling out checklists. Medicine is an art as much as a science; that’s why to become a doctor takes over a decade. There aren’t enough checklists in the world to ensure good medical care.
Checklists in medicine evolved initially to keep insurance companies from denying payments for alleged lack of documentation and to help fend off lawsuits. The problem with checklists is that they are often used as excuses to allow less expensive (and less trained) personnel to provide care. Moreover, the checklist recepients have become immune to paying attention to the lists due to checklist information overload. And it’s not just checklists – All day long our fax machine and computer are spitting out voluminous computer-generated notes from doctors’ offices describing five minute visits for minor medical problems.
What we need in medicine is less time checking lists and more time for more qualified people to think and analyze. People need to get up out of their seats and away from their computers and to communicate the old-fashioned way – by talking.
In Dallas the hospital initially acknowledged that a nurse took a travel history and filled out a checklist, but the information never made it to those responsible for the care of the patient. Their most recent explanation as reported on CNN is “As a standard part of the nursing process, the patient’s travel history was documented and available to the full care team in the electronic health record, including within the physician’s workflow,” In other words blame now is being shifted from the nurse (her job ended when she put the travel checklist into the computer) to the “full care team”. Using the term “full care team” might be an artful way of saying the patient wasn’t actually seen by a doctor, but rather by a nurse practitioner or physician assistant.
Regardless of who saw the patient it is tempting to try to put the blame on the nurse, or the doctors, or conclude that their computer system just needs an upgrade to better flag alarming issues. The real problem is the electronic checklist mentality which is overtaking medicine. And though the bean counters would like us to believe that good medicine can be quantified and accomplished by more and more computerization, this should serve as a wake-up call to the contrary.
Until next week this is Dr. Ed Taubman primary care Olney MD 301-774-5400 where friendly and helpful people are ready to serve you and the doctor hasn’t forgotten how to pick up the phone to coordinate your care with your other health care providers.
 Congestive heart failure can be a serious ailment leading to shortness of breath, fluid retention, and early death. About 2% of adults are diagnosed with this condition; and for those 65 and over 6-10% are affected. The most common causes are heart damage due to heart attack and blocked arteries but other conditions such as leaky valves, viral infections, and inherited conditions can also be causative. As a damaged heart continues to pump its undamaged tissue can get overworked and eventually wear out. As a result congestive heart failure tends to get worse with time. Treatments for this condition date back to over two hundred years ago with the introduction of digitalis, a derivative of the foxglove plant. Although digitalis was the mainstay of treatment for centuries, modern studies have shown that digitalis, while making patients feel better, did not prolong longevity.
Congestive heart failure can be a serious ailment leading to shortness of breath, fluid retention, and early death. About 2% of adults are diagnosed with this condition; and for those 65 and over 6-10% are affected. The most common causes are heart damage due to heart attack and blocked arteries but other conditions such as leaky valves, viral infections, and inherited conditions can also be causative. As a damaged heart continues to pump its undamaged tissue can get overworked and eventually wear out. As a result congestive heart failure tends to get worse with time. Treatments for this condition date back to over two hundred years ago with the introduction of digitalis, a derivative of the foxglove plant. Although digitalis was the mainstay of treatment for centuries, modern studies have shown that digitalis, while making patients feel better, did not prolong longevity.
Over the last 30 years there has been incremental progress in the treatment of this condition as researchers have gradually better understood the underlying mechanisms contributing to worsening heart failure. The addition of drugs such as ACE inhibitors and ARB inhibitors, which are widely used to treat hypertension, and diurtetics such as spironolactone have proven useful in extending life and reducing symptoms. Mechanical devices like resynchronization pacemakers and automatic defibrillators, which shock the heart out of fatal irregular heart beats, have found their places in the management of congestive heart failure as well. More recently beta blockers, a class of drugs which had been avoided for years in heart failure because of concerns that they would weaken the heart, are now widely used; studies have shown that they can actually help protect the heart from further damage. Heart transplantation has proven to be an imperfect solution given the growing numbers of people with congestive heart failure and the considerable challenges to perfecting a safe and effective mechanical heart have yet to be overcome.
A new study reported last week in the “New England Journal of Medicine” reports on a new drug, LCZ696, part of a new class of medicines collectively known as angiotension receptor-neprilysin inhibitors. Combined with a traditional ARB drug valsartan, this new drug was studied in a group of over 8000 patients with heart failure; half received the new combination and the other half received standard treatments. Over a study period of more than two years, there was a 13% decrease in death, a 21% decrease in hospitalizations, and an accompanying significant improvement in symptoms. This study is a tribute to the international collaboration of researchers and the participating patients and will likely usher in a new era in the treatment of this ailment.
Dr. Ed Taubman Primary Care Olney, MD 301-774-5400
Know someone who is looking for a great primary care practice? We are now accepting new patients!
Click Here to start receiving my weekly health blog post via email – It’s Free!
 When and whom to test for a genetic predisposition to cancer has been confusing to both patients and many doctors. The traditionally high cost of testing (thousands of dollars), coupled with insurance companies’ reluctance to pay for testing in the general population, has led to a mystique that such testing is both unnecessary and unaffordable to most people. However, there is one group that seemingly would be ripe for such testing – an ethnic group that has ten times the chance of carrying a genetic mutation that, when present, can cause an 80% lifetime risk of breast cancer and more than a 40% lifetime risk of ovarian cancer. Furthermore, because of a genetic concept known as founder mutations, the cost of doing genetic testing in this population is about a tenth what it would normally be.
When and whom to test for a genetic predisposition to cancer has been confusing to both patients and many doctors. The traditionally high cost of testing (thousands of dollars), coupled with insurance companies’ reluctance to pay for testing in the general population, has led to a mystique that such testing is both unnecessary and unaffordable to most people. However, there is one group that seemingly would be ripe for such testing – an ethnic group that has ten times the chance of carrying a genetic mutation that, when present, can cause an 80% lifetime risk of breast cancer and more than a 40% lifetime risk of ovarian cancer. Furthermore, because of a genetic concept known as founder mutations, the cost of doing genetic testing in this population is about a tenth what it would normally be.
The ethnic population I am speaking about are people of Jewish descent from eastern Europe and Russia – the so-called Ashkenazi population which encompasses almost all Jewish people in the United States. And while this group would seem to be the perfect genetic storm of high chance of carrying a mutation, high risk of life threatening disease, and relatively low cost to testing, it is also in my experience the perfect storm for excuses not to test: “Nobody in my family has it”, “My insurance won’t cover it”, “I’ll lose my insurance if I am a carrier”, “I would never have my breasts removed”, “I’ve already had cancer”, “I’m too old to do anything about”, “I’m too young to think about it.”
A recent study conducted in Israel has brought to public attention what some of us in the field of cancer genetic testing have been saying for years: If you are of Jewish descent, even if you don’t have a personal or family history of breast or ovarian cancer, you should consider being tested for the BRCA1 and BRCA2 founder mutations. (BRCA1 refers to the first discovered breast cancer associated gene and BRCA2 for the second such discovered gene).
Yet what difference would it make, you ask? Most people’s thoughts about BRCA are focused on breast cancer risk. Understandably, many women who are fine now are reluctant to consider genetic testing and contemplate prophylactic mastectomies to prevent a breast cancer they may or may not get in the future, due to a genetic mutation. Nonetheless, BRCA women carriers have other options when it comes to reducing breast cancer risk and younger women who carry mutations should afford themselves of screening starting at age 25 with MRI as a complement to mammography. However, the even more compelling reason to be tested is the inordinately high risk of ovarian cancer in this population.
As shown above, the lifetime risk of ovarian cancer in BRCA carriers in the Israeli study was over 50% and starts to dramatically rise in their mid forties. Unfortunately, there is NO effective screening for ovarian cancer; but having one’s ovaries removed after having your family effectively prevents ovarian cancer. Today, laparoscopic or robotic removal of the ovaries is a relatively simple surgical procedure with a quick recuperation.
As summarized by the study authors: “We determined that risks of breast and ovarian cancer for BRCA1 and BRCA2 mutation carriers ascertained from the general population are as high as for mutation carriers ascertained through personal or family history of cancer. General screening of BRCA1 and BRCA2 would identify many carriers who are currently not evaluated and could serve as a model for population screening for genetic predisposition to cancer.”
Today we live in an age called “evidence based medicine” whereby, even if something is obvious on the face of it, one must do a study to prove it is true before it can become accepted medical practice for which insurance companies will pay. This study both provides such evidence and has increased public awareness of the benefits of cancer predisposition testing. It also opens the door to insurance companies offering universal testing of BRCA in the Jewish Ashkenazi population even when there is no known family history of breast or ovarian cancer.
So, to all my friends of the Jewish faith who are in synagogue this week celebrating the coming of the Jewish New Year, take a look around. One in forty of you carries a genetic tendency that began over 2000 years ago and through both men and women has been passed down from generation to generation as are the biblical passages you are reading about. This is one case where we have the potential to alter our genetic destiny – so consider BRCA counseling and testing in the New Year to come; even if no one in your family has had breast or ovarian cancer and your insurance company is stingy. Then pen a letter to your insurance company and your benefits manager inquiring why one of the most cost-effective and life-saving tests we can offer is not routinely covered in this high risk population.
by Dr Ed Taubman Olney Maryland 301-774-5400
General Internal Medicine and Cancer Genetic Counseling
 We just had our open house for our next multidisciplinary integrative weight loss program which begins on September 29. We heard the testimonials of recent participants who had struggled with weight for most of their lives until we helped them re-engineer their relationship with food and healthy eating. Hearing their inspiring stories of lifelong struggles and that some had now lost 30 or even 40 pounds through simple changes in diet is exciting for our integrated weight loss team (nutritionist, psychotherapist, chef, yoga/personal trainer, and physician). Recently, we were approached to create a similar program directed to obese teens and will be working with a local group in Olney to create an effective program for adolescents.
We just had our open house for our next multidisciplinary integrative weight loss program which begins on September 29. We heard the testimonials of recent participants who had struggled with weight for most of their lives until we helped them re-engineer their relationship with food and healthy eating. Hearing their inspiring stories of lifelong struggles and that some had now lost 30 or even 40 pounds through simple changes in diet is exciting for our integrated weight loss team (nutritionist, psychotherapist, chef, yoga/personal trainer, and physician). Recently, we were approached to create a similar program directed to obese teens and will be working with a local group in Olney to create an effective program for adolescents.
The epidemic of adult and childhood obesity, diabetes, and chronic illnesses makes one question if what we are doing is working. Like all issues in health and medicine, our nutritional thinking has changed dramatically over the years as our scientific knowledge has advanced. But, are the servings of the school cafeteria today much different from what you and I grew up with? This thought-provoking article about a New York Elementary School That Is Changing More Than Meals http://nblo.gs/ZGkeC got me thinking about the right time to teach the next generation about changes in nutritional thinking. Please read it and then come back and take my poll below to share what you think![polldaddy poll=8298499]
 Recently there have been some new articles concerning the benefits, and perhaps downsides, of limiting one’s salt (sodium chloride) intake. We know that high salt in one’s diet can contribute to high blood pressure. We know that people who have heart problems such as congestive heart failure, hypertension, or severely impaired kidney function may need to limit their salt intake. We know that countries in the world that have the highest salt intake often have the highest rates of cardiovascular disease. So it would seem logical to infer that, globally, if we all lowered our salt intake, there would be a reduction in cardiovascular complications such as heart attacks and stroke.
Recently there have been some new articles concerning the benefits, and perhaps downsides, of limiting one’s salt (sodium chloride) intake. We know that high salt in one’s diet can contribute to high blood pressure. We know that people who have heart problems such as congestive heart failure, hypertension, or severely impaired kidney function may need to limit their salt intake. We know that countries in the world that have the highest salt intake often have the highest rates of cardiovascular disease. So it would seem logical to infer that, globally, if we all lowered our salt intake, there would be a reduction in cardiovascular complications such as heart attacks and stroke.
With that in mind, the American Heart Association and the CDC have recommended a very low (2.3 grams of sodium per day or less) diet for all. If you are over the age of 50, African American, hypertensive, or diabetic, they recommend further limiting your total sodium intake to 1.5 grams or less. To keep that in perspective, the average American takes in more than twice that amount (3.4 grams according to the CDC). For most people about a quarter of their sodium intake comes from the salt shaker and three quarters from “processed foods” including most canned vegetables, soups and sauces; these have added sodium, which enhances taste and texture, and acts as a preservative. Ditto for breads and rolls. Fresh and processed poultry and cold cuts are typically high in salt content as well. Restaurant foods and, of course, potato chips and pretzels are sources of excess salt and sodium.
Preventing cardiovascular disease is certainly a worthwhile endeavor. Unfortunately, when subjected to scientific scrutiny, many commonly accepted preventative interventions other than lifestyle change such as exercise and keeping one’s weight down have failed to live up to their promises. In previous posts we have addressed controversies about the roles of daily aspirin, saturated fats, vitamin D and others in preventing disease and prolonging life. So what about those recent articles about salt and health?
They do confirm that with higher levels of sodium intake (greater than 6 grams per day), there indeed is a higher risk of cardiovascular disease and hypertension. However, one of the articles suggests that for the average person the ideal range of salt intake might be more in the order of 3 to 6 grams per day; and for those who significantly lower their salt intake down to the levels recommended by the American Heart Association there may actually be an increase in cardiovascular disease. The same article also confirmed previously noted trends that higher intake of potassium (as commonly found in fruits and vegetables) may help to reverse some of the adverse effects of salt.
While the experts continue to debate the true meaning of these articles, and look to confirm or refute their findings, what are the prudent actions to take?
First, try and take an inventory of how much salt you consume on average. Learn to read labels.
If your daily salt intake is 6 grams a day or more, all the studies indicate that your health is potentially being jeopardized; and you should strive to reign in your salt intake. If you do need to be on a lower salt diet studies have shown that people are much more successful if another family member consumes the same diet.
Try and increase your fruits and vegetables which will help keep your potassium levels up and also help you keep your weight in check.
If you are healthy and without hypertension or heart failure, given the above noted controversy among the “experts,” you don’t necessarily need to go on a very low sodium diet – unless directed to do so by your doctor – but continue to exercise, keep your weight down, and improve on your intake of fruits and vegetables.
Remember, everyone is different and what is best for one person might not be best for you. The “experts” who make the general recommendations for the population at large aren’t taking care of you personally. If in doubt check with your own doctor.
By Dr Ed Taubman Olney Maryland 301-774-5400
Looking for a high quality primary care practice? We are now accepting new patients
Looking to lose weight? The next session of our acclaimed weight loss program starts soon – click on “Integrative Weight Loss Solutions” above for more details
 The past three decades have seen many incremental advances in the diagnosis and treatments for viral hepatitis. When I started practice, the only commonly identified causes of viral hepatitis were types A, which typically is short-lived and without long term ill effect, and hepatitis B, which can cause chronic liver problems and liver cancer. Hepatitis B cases in this country have been steadily dropping since the introduction of an effective vaccination series which is now started at birth. Unlike hepatitis A and B there are no vaccinations to prevent hepatitis C. For a number of years now, we have had a test to identify hepatitis C. The initial benefit of having a test to identify hepatitis C was to protect the blood supply which prevented transmission from blood transfusions thereby starting a slow decline in the number of new cases. However, as more and more people have been tested, we now know that as many as 3 million Americans, predominantly baby boomers, may be carrying the virus; and most people who carry the virus are not aware of it.
The past three decades have seen many incremental advances in the diagnosis and treatments for viral hepatitis. When I started practice, the only commonly identified causes of viral hepatitis were types A, which typically is short-lived and without long term ill effect, and hepatitis B, which can cause chronic liver problems and liver cancer. Hepatitis B cases in this country have been steadily dropping since the introduction of an effective vaccination series which is now started at birth. Unlike hepatitis A and B there are no vaccinations to prevent hepatitis C. For a number of years now, we have had a test to identify hepatitis C. The initial benefit of having a test to identify hepatitis C was to protect the blood supply which prevented transmission from blood transfusions thereby starting a slow decline in the number of new cases. However, as more and more people have been tested, we now know that as many as 3 million Americans, predominantly baby boomers, may be carrying the virus; and most people who carry the virus are not aware of it.
Though most people with hepatitis C never develop serious complications, an important minority develop cirrhosis, liver failure, or liver cancer. Until late stage complications arise, the infection is usually asymptomatic; and usual liver blood tests are either normal or show low grade abnormalities that may be falsely attributed to medications that the person is taking. Though progress in the treatment of hepatitis C up to now has been remarkable, many of the treatments have been less than optimal. They can take almost a year, require a weekly injection plus as many as 18 pills per day for treatment of the infection and the side effects from the medications, and be accompanied by unpleasant side effects – with cure rates between 40 and 80% depending on the strain with which one is infected.
With the recent advent of two new medications, Olysio (simeprevir) and Sovaldi (sofosbuvir), we appear to be quickly entering a new era in the treatment of this potentially serious condition. In some cases treatment can now be as short as 12 weeks with pills only and with significantly fewer side effects and cure rates of over 90%.
An analysis of recent trends published in the Annals of Internal Medicine suggests that in the United States alone, with the adoption of universal hepatitis C screening, almost a million new candidates for treatment could be identified. With the wide- scale adoption of the newer treatments, the disease could become a rarity in the next twenty years, preventing over a quarter million liver-related deaths.
The new drugs, though, come with a steep price; $1000 per pill with an average estimated cost of $84,000 per treatment and a growing debate over a fair price for breakthrough drugs that are the culmination of decades of research that can prevent costly medical complications in years to come. Plus, in a time of strained health care budgets, who will pay the many billions of dollars for the treatments in this country and in poorer developing countries?
Wish to know your hepatitis C status? The easiest way is to donate blood – since 1992 all donated blood is screened and you would be notified if infected. Haven’t donated blood or ever been tested? Let us know at the time of your physical and we can include a hepatitis C blood test with your complete blood work and cholesterol tests.
By Dr Ed Taubman Olney Maryland 301-774-5400
Looking for a high quality primary care practice? We are now accepting new patients
Integrative Weight Loss Solutions Launched On April 21. Our first group of 25 participants lost an average 24 pounds over twelve weeks while eating regular foods, without supplements or gimmicks, learning how to eat healthy, get moving, and having fun in the process!
Thanks to all who attended our open house on September 8 and to our program participants who spoke including Restauranteur Barry Schwartz who told how he has lost forty pounds and counting through our program and Debbie Butler and Husband Rick who have lost together 60 pounds and counting. Our next 10 week session will begin on Monday September 29. There are still a few slots available – you can reserve your spot by filling out the form below.
“Thank you for the Time and effort you all have put in to make a miracle happen in my life. While over 20 pounds in 7 weeks may not sound a lot to some, To me, who has never lost weight on a diet, this was a life changing event. Thanks for the help with cooking, yoga and mental discipline.” Shiela Hanson Cloverly MD
Program Participants
Author Nutritionist Rick Weissinger RD, MS, CPT
Yoga Instructor & Personal Trainer Kathi Doan (giving Yoga Instructions above)
Psychotherapist Andrea Lopes LCSW-C (demonstrating chair yoga above)
Washingtonian Top Doctor Edward Taubman, M.D.
Local Chef Debbie Amster Recently Featured On Local TV
Our Ten Week Program Meets Weekly From 7:00 to 8:30PM At The Olney Counseling Center at 3430 North High Street
Topics Covered Include
Re-Engineering Your Food Intake – What Should We Be Eating?
Emotional Eating – Identify Your Triggers And Develop Strategies To Manage Them
Get Moving And Relax – Yoga Techniques to Help You Win The Battle
Learn To Cook And Eat Healthy With Cooking Demos And Trips To The Grocery Store
At The Olney Counseling Center 3430 N High Street, Olney MD
Participation Is Limited To approx 25 people.
The present cost for the initial ten week program is $599 (patients of Dr Edward Taubman and Members of OlneyMyWellness receive a $100 discount).
Call 301-774-5400 for More Information or Fill Out the Form Below
[si-contact-form form=’5′]
 Once again prostate cancer screening has been in the news – fueled by a provocative book written by Dr. RJ Ablin entitled “The Great Prostate Hoax: How Big Medicine Hijacked the PSA Test and Caused a Public Health Disaster”. Dr. Albin’s claims are not easily dismissed as he is the person who discovered PSA in the 1970s. Dr. Albin’s discovery of PSA, and its initial FDA approval, was for the purpose of following men who were seemingly cured of prostate cancer, and to alert doctors that the cancer might be coming back and thus require additional treatment.
Once again prostate cancer screening has been in the news – fueled by a provocative book written by Dr. RJ Ablin entitled “The Great Prostate Hoax: How Big Medicine Hijacked the PSA Test and Caused a Public Health Disaster”. Dr. Albin’s claims are not easily dismissed as he is the person who discovered PSA in the 1970s. Dr. Albin’s discovery of PSA, and its initial FDA approval, was for the purpose of following men who were seemingly cured of prostate cancer, and to alert doctors that the cancer might be coming back and thus require additional treatment.
However, ultimately the test started to be used for the early detection of prostate cancer in men who had no symptoms. Unfortunately, when used for that purpose, the PSA is a very imperfect test. According to Dr. Albin, in a recent interview with Medscape, the test is wrong 80% of the time as a predictor to see if an otherwise healthy appearing man has prostate cancer. This is similar to the situation in ovarian cancer where the CA-125 blood test is used by cancer specialists to follow and treat women who have ovarian cancer; unfortunately it has failed to be an effective test in catching early ovarian cancer.
Dr. Albin highlights some of the issues of using the test for widespread screening: “A man can have a PSA of 0.5 ng/mL and have cancer, or a PSA of 11 ng/mL and not have cancer…..Furthermore prostate cancer is an age-related disease. If you get, for example, 100 men — black or white — between the ages of 60 and 69 years and do biopsies, you will find that 65% of these men have prostate cancer because it’s age-related.”
Importantly the Achilles heel of the test is that it is unable to make the important distinction as to which men have a slow moving cancer that they will outlive and would be best ignored, and which men are destined to have a much more aggressive and ultimately life – threatening cancer.
Dr. Albin argues that, as a result of the misuse of his test, an unstoppable multi-billion dollar industry has developed where men are tested routinely, many are found to have elevated PSA results, countless have prostate biopsies, and many have removal of their prostates with not infrequent side effects such as sexual impotence and loss of urinary control; all at the cost of billions of health care dollars with few if any lives saved to show for it. He calls robotic surgery “a train that is ready to come off the tracks;” and that when the FDA approved robotic surgery for the prostate, its approval was not based on any human studies.
Supporters of routine PSA testing point to a long term European study with a 20% decrease in deaths due to PSA screening. Detractors point to the largest ongoing US study which find few, if any, lives saved.
So where does that leave us presently in 2014?
The PSA test is clearly a far from perfect test for the detection of early prostate cancer. There can be real harms to testing but possibly a small benefit in lives saved. However, the benefits of testing are not as clear as, say, mammography for early breast cancer detection in women, or as noted in my recent post the benefits of universal colonoscopies for the prevention of colon cancer. Unfortunately, when it comes to prostate cancer, there is no better test on the horizon. According to Albin that may in part be due to the fact that we spend over 3 billion dollars a year on PSA screening, but the National Cancer Institute spends just one tenth that on urological research.
Finding the right doctor isn’t easy—and it shouldn’t be. You are putting your life, and health, in someone else’s hands. You need to feel confident that this person is skilled and qualified enough to give you the care you deserve. You should “shop” for a doctor the same you would a lawyer or even a good mechanic. Your relationship with your primary care doctor is one of the most important professional relationships you will develop.
People spend more time shopping for a new car than they do “shopping” for the right primary doctor. A primary care doctor helps keep you healthy and provides a “home base” for all of your medical needs. Knowing what to look for when selecting a new doctor is critical. Here are a few things to remember when searching for a new doctor in Olney, Maryland.
Call around to several different doctors’ offices. Don’t stop at the very first doctor you find on Google. Consider your choices. Is the phone answered by a live, friendly, caring person? Remember you need a friendly and competent staff to help you wind your way through the complicated web of medical care to get appointments, schedule tests, fill prescriptions, and handle insurance properly. The quality of the staff you encounter tells you a lot about the quality of the doctor and the medical services you will receive.
Ask for references! Talk to family, friends, and co-workers and see what primary doctor they chose. Is the doctor rated Top Doctor? When checking references on the internet, ask yourself are there enough reviews to accurately reflect on the doctor. Look for ratings that have over fifty reviews.
Ask about the doctor’s credentials. You should always make sure your doctor has credentials and is properly licensed. A Board Certified Internist is an expert in the field of adult medicine. Did you know that cardiologists, endocrinologists, gastroenterologists, and cancer specialists have to become board certified internists first? Did you know that internists are known for being excellent diagnosticians and are commonly known as the doctors that other doctors go to? And don’t forget about the credentials of their staff; more and more primary care practices have replaced experienced seasoned registered nurses with years of training with medical assistants who have had just a few weeks of training.
Talk to your doctor about insurance plans. Does the doctor accept Medicare? If you use out of network benefits, are they discounted through a service such as PHCS or Multiplan which can save you a lot of out- of- pocket money? It is more and more common for doctors to charge an extra fee to keep their practices smaller and manageable and to retain experienced staff. Having a doctor who doesn’t see as many patients gives you the ability to receive same day appointments and for him to spend more time taking care of you.
Look for a doctor who has good bedside manner. You don’t want a doctor who just comes into the room, tells you that you have something wrong, gives you a prescription and then walks out. You also don’t want to be the one always telling your doctor what to do. You want to look for a doctor who will take the time to sit down with you and discuss all of your health concerns and all of the possible treatments. Good medical care is a partnership.
Make sure your doctor’s approach to healing is consistent with your views and philosophies and that he is an expert in his field. Does your doctor have a holistic approach to your health? Your doctor should share the same beliefs you have on the body and healing. Does your doctor write a medical blog or conduct “Grand Rounds” at local hospitals to educate other doctors?
Do you get to see your doctor? In many practices, particularly those run by large entities such as hospitals, you may be seen most of the time by a physician assistant or nurse practitioner. Be mindful that these non-physicians have a fraction of the training and experience of a Board Certified Internist. This can result in important diagnoses being missed or delayed, or the reverse – unnecessary testing.
It is important to consider the kind of care you are looking for and where you are looking to get that care. Everyone should spend time “shopping around” for a primary care doctor to find the right fit. Making the right, lasting relationship with your doctor is important for long-term quality health care.
If you are in the Olney, Maryland area, schedule a time to visit with Dr. Edward Taubman. Dr. Taubman will spend time with you discussing your health history and take the time to get to know you. Dr. Taubman has repeatedly been rated “Top Doc” by “Washingtonian” and “Checkbook” magazines. Go to zocdoc.com to read over 200 reviews on Dr Taubman who has a rating of 4.9 out of 5.0 Dr. Taubman has been repeatedly invited to lecture at local area hospitals including Medstar Montgomery General, Holy Cross, Shady Grove, Mercy Baltimore, and Medstar Franklin Square. Schedule an appointment online, or call Dr. Taubman today at 301-774-5400
 Most cases of breast cancer can not be attributed to a specific cause. It is theorized that the majority of breast cancer is due to incompletely understood interactions between environmental exposures and relatively weak genetic influences and one’s lifestyle; such as exercise and the foods we eat. However, in an important minority of patients a strong genetic influence can sometimes be found. The best known such strongly inherited influences are genetic changes in the BRCA1 and BRCA2 genes. The role of these genes in the development of breast, and ovarian cancers, has been known since the 1990s. However, there remain many families who have strong family histories in which BRCA testing has been uninformative. This had led to speculation that a “BRCA3” gene may yet be discovered. Though a search for a so called BRCA3 gene has been underway for many years a new study reported in the New England Journal of Medicine indicates that a gene called PALB2 may play a more prominent role in causing breast cancers in some families than had previously been appreciated.
Most cases of breast cancer can not be attributed to a specific cause. It is theorized that the majority of breast cancer is due to incompletely understood interactions between environmental exposures and relatively weak genetic influences and one’s lifestyle; such as exercise and the foods we eat. However, in an important minority of patients a strong genetic influence can sometimes be found. The best known such strongly inherited influences are genetic changes in the BRCA1 and BRCA2 genes. The role of these genes in the development of breast, and ovarian cancers, has been known since the 1990s. However, there remain many families who have strong family histories in which BRCA testing has been uninformative. This had led to speculation that a “BRCA3” gene may yet be discovered. Though a search for a so called BRCA3 gene has been underway for many years a new study reported in the New England Journal of Medicine indicates that a gene called PALB2 may play a more prominent role in causing breast cancers in some families than had previously been appreciated.
Testing for PALB2 is now more readily available. For those families where multiple family members have had breast cancer, and previous BRCA testing has been uninformative, PALB2 testing may in some cases provide an answer. Knowing the genetic cause in a breast cancer prone family can help women better understand who in a family may be at particularly high risk and need to take special precautions; and who is at more average risk. Dr Taubman is a graduate of the National Cancer Institute funded program in cancer genetics at the City of Hope and is able to help patients make informed decisions about the role of cancer genetic testing, help obtain insurance coverage as appropriate, and offer advice on preventative strategies.
 Integrative Weight Loss Solutions Launched On April 21. Our first group of participants have lost an average 24 pounds over twelve weeks while eating regular foods, without supplements or gimmicks, learning how to eat healthy, get moving, and having fun in the process!
Integrative Weight Loss Solutions Launched On April 21. Our first group of participants have lost an average 24 pounds over twelve weeks while eating regular foods, without supplements or gimmicks, learning how to eat healthy, get moving, and having fun in the process!
[easychart valuenames=”Week 2, 3, 4, 5, 6, 7, 8, 9, 10,11,12″ group1values=”1.5,3.0,4.5,6.0,7.5,9.0,10.5,12.0,13.5,15,16.5″ group2values=”3.99,8.81,9.09,11.0,13.8,15.4,16.7,17.5,19.5,21.43,23.36″ groupnames=”Goal, Present Group” ]
Program Participants
Author Nutritionist Rick Weissinger RD, MS, CPT
Psychotherapist Andrea Lopes LCSW-C
Yoga Instructor & Personal Trainer Kathi Doan
Washingtonian Top Doctor Edward Taubman, M.D.
Local Chef Debbie Amster Recently Featured On Local TV
Our Ten Week Program Meets Weekly From 7:00 to 8:30PM At The Olney Counseling Center at 3430 North High Street
Topics Covered Include
Re-Engineering Your Food Intake – What Should We Be Eating?
Emotional Eating – Identify Your Triggers And Develop Strategies To Manage Them
Get Moving And Relax – Yoga Techniques to Help You Win The Battle
Learn To Cook And Eat Healthy With Cooking Demos And Trips To The Grocery Store
At The Olney Counseling Center 3430 N High Street, Olney MD
Participation Is Limited To approx 25 people.
The present cost for the initial ten week program is $599 (patients of Dr Edward Taubman and Members of OlneyMyWellness receive a $100 discount).
Those who wish to can then join our weekly maintenance program
Call 301-774-5400 for More Information or Fill Out the Form Below
[si-contact-form form=’5′]
 For most women routine pelvic examinations by their internist, family doctor, or gynecologist have become annual rituals. However, some recent recommendations have raised questions about the value of these exams and in the process confused many patients and physicians alike. Much of the confusion has to do with the terms “Well Woman Exam, PAP test, and “pelvic examination”. For most women these terms are synonymous. However, in the medical field they can be three separate things.
For most women routine pelvic examinations by their internist, family doctor, or gynecologist have become annual rituals. However, some recent recommendations have raised questions about the value of these exams and in the process confused many patients and physicians alike. Much of the confusion has to do with the terms “Well Woman Exam, PAP test, and “pelvic examination”. For most women these terms are synonymous. However, in the medical field they can be three separate things.
A PAP test, for instance, is a swab taken from the entrance to the uterus or womb. The purpose of the PAP test is to check for either early changes that could lead to cervical cancer, or the detection of the Human Papillomatous Virus (HPV) that causes the vast majority of cervical cancer. A PAP test requires a woman to be on an exam table, legs up in stirrups, with the insertion of a device known as a speculum which opens the vagina so that the cervix can be seen and the PAP smear of the cervix done.
A “Pelvic Exam” (sometimes called an “Internal”) starts out also with a woman up in stirrups. However, instead of inserting a speculum to visualize the cervix, this procedure involves the insertion of one gloved hand in the vagina and the other on the abdomen to feel if anything in between seems abnormally enlarged such as the uterus or ovaries.
A “Well Woman Exam” literally means an otherwise well woman visiting the doctor, discussing important issues such as heart health, diabetic tendency, osteoporosis screening, blood pressure checking, having a breast exam, and otherwise being appropriately examined which may or may not include a PAP smear being obtained or a pelvic exam.
The recent brouhaha which has caused all the confusion is really only about the value of that second element – the “Pelvic Exam” in otherwise healthy, non pregnant, asymptomatic women. Turns out that poking around with one hand in the vagina and the other on the abdomen rarely finds anything serious and occasionally results in surgery that in retrospect might not have been necessary.
That’s not to say that a pelvic exam couldn’t disclose factors of interest or importance to the patient or doctor such as the presence of non – cancerous “fibroids” or bladder “prolapse” – which might contribute to incontinence. Trying to catch early ovarian cancer is often cited as a reason to do routine pelvic exams. Unfortunately, repeated studies have shown that ovarian cancer is rarely detected on routine pelvic examination; for that matter there does not exist any reliable test for detecting early ovarian cancer in women who have no symptoms.
So, what does this mean for the average woman? The most important thing to understand is that women who are feeling well should still see the doctor from time to time to check their blood pressure, cholesterol, breasts, skin, and thyroid; and have referrals for preventative health measures as may be appropriate based on their family history and age, such as mammograms, bone density tests, and colonoscopies.
Women, between the ages of 21 and 65 still should have periodic PAP tests which still involves getting up on the exam table with legs up in stirrups. Current guidelines for women without symptoms and previously normal PAP tests support PAP testing every three years – though as newer technology to test for HPV is introduced, the recommended frequency for some women may decline.
So, in summary, should women give up going to the doctor for a well woman exam? Absolutely not.
Should women younger than 65 give up on PAP smears? Absolutely not.
Should all women regardless of age have an annual pelvic exam/”Internal”?? Not necessarily. However, keep in mind that part of the debate in medical circles revolves around the question as to how often doing the exam results in finding something significant in people who otherwise feel well. Part of the debate also revolves around cost effectiveness. The same argument could be made for not listening to people’s hearts with a stethoscope, or not listening to their lungs as that might result in further testing such as echocardiograms, chest xrays or CT scans without proof that doing so results in longer lives.
Importantly, none of this applies to women who have symptoms that could be warning signs such as abnormal bleeding, unexplained bloating or pains. If these persist, they require a complete exam regardless of age.
by Dr Ed Taubman Primary Care Physician Olney MD 301-774-5400
Once Again Voted Top Doctor “Washingtonian Magazine”
To Join my Health Blog and start receiving weekly e-mails of new informative posts click here
Follow me on fB facebook/olneymywellness
 The balance between HDL – the so – called “Good or Happy” cholesterol and LDL – the so – called “Lousy” cholesterol is often used as a way to evaluate one’s risk of developing clogged arteries. However, some people still have heart attacks or strokes despite seemingly ideal levels of of these fats in their blood, while others with low HDL and high LDL levels seem to do just fine.
The balance between HDL – the so – called “Good or Happy” cholesterol and LDL – the so – called “Lousy” cholesterol is often used as a way to evaluate one’s risk of developing clogged arteries. However, some people still have heart attacks or strokes despite seemingly ideal levels of of these fats in their blood, while others with low HDL and high LDL levels seem to do just fine.
So researchers have been searching for different kinds of blood tests to better define one’s risk of getting clogged arteries and better treatments for those at risk. One potential way to better define one’s risk for heart attack or stroke is the use of blood tests that look at more than just HDL, LDL, and triglycerides. In our practice we also are integrating newer tests with names such as LDL particle number, HDL Map, and LDL pattern, just to name a few.
The mainstay of cholesterol drug treatment, the class of drugs known as statins, while safe and effective for most, can be difficult for some people to tolerate because of muscle pains or even weakness. Niacin, which has been around for a long time and can increase the good HDL, has yet to show that it is beneficial when it comes to lowering one’s risk of arteriosclerosis. Similarly, drugs known as fibrates (tricor, lopid) have struggled to show they reduce arteriosclerosis. Ditto for Zetia. New drugs that raise HDL have not come to market because of safety concerns.
The one class of drugs that may soon reach the market are the PCSK9 inhibitor drugs. These drugs work on something called LDL Receptor Metabolism and can lower “lousy” cholesterol levels dramatically. They have the potential to be game changers in the treatment of high cholesterol and to manage those who already have clogged arteries by dropping LDL levels to previously unimaginably low levels. One drawback: they would need to be given by injection, but perhaps once a month would be sufficient.
Is lowering one’s cholesterol so low safe? The PCSK9 inhibitor drugs are modeled on the fact that a few people have been discovered with genetic variations in their PCSK9 genes that naturally lower their LDL levels from a typical 130 or so to only 15! These people seem to be otherwise healthy and without any signs of arteriosclerosis. With cholesterol levels pushed down that low, it is is conceivable that this class of drugs might not only slow down arteriosclerosis, as do present statin drugs, but might actually reverse it. Nonetheless, if approved by the FDA, it may well take years of experience to know for sure that the drugs don’t have unintended consequences. More than three decades after approval, we are still learning about the pros and some of the cons of statins. In the meantime lifestyle changes such as weight loss and increased exercise as taught in our multidisciplinary weight loss program can make a big difference for many people in both their cholesterol numbers and their cardiovascular risks, and statins will remain an important treatment for some time to come.
by Dr Ed Taubman Primary Care Physician Olney MD 301-774-5400
Once Again Voted Top Doctor Washingtonian Magazine
To Join my Health Blog and start receiving weekly e-mails of new informative posts click here
Follow me on twitter @askDrTaubman
Follow me on fB facebook/olneymywellness

 Despite the fact that as a country we spend much more on health care than anyone else in the world, we lag in health care measures when compared to others. Medicare spends over a half trillion dollars each year, and you can’t blame them for trying to figure out how to lower costs and make sure that the care they are paying for is actually promoting health. One such attempt is the advent of accountable care organizations or ACOs. In Maryland there are presently over a dozen of these groups which have formed, and almost every physician or hospital will soon be part of one of them. We are members of a Medicare certified ACO known as Maryland Collaborative Care which was originally formed by the Maryland State Medical Society. We have researched them and so far are very pleased to partner with Maryland Collaborative Care. Some of you may have received a letter from Medicare about our participation in Maryland Collaborative Care, giving you the choice to allow this ACO to view where your health care dollars are being sent. Once Maryland Collaborative Care ACO has that information, it can share it with us; and we can work together to help you stay healthy.
Despite the fact that as a country we spend much more on health care than anyone else in the world, we lag in health care measures when compared to others. Medicare spends over a half trillion dollars each year, and you can’t blame them for trying to figure out how to lower costs and make sure that the care they are paying for is actually promoting health. One such attempt is the advent of accountable care organizations or ACOs. In Maryland there are presently over a dozen of these groups which have formed, and almost every physician or hospital will soon be part of one of them. We are members of a Medicare certified ACO known as Maryland Collaborative Care which was originally formed by the Maryland State Medical Society. We have researched them and so far are very pleased to partner with Maryland Collaborative Care. Some of you may have received a letter from Medicare about our participation in Maryland Collaborative Care, giving you the choice to allow this ACO to view where your health care dollars are being sent. Once Maryland Collaborative Care ACO has that information, it can share it with us; and we can work together to help you stay healthy.
The theory behind ACOs is that by their promoting information sharing among physicians and hospitals and providing targeted extra resources, you can receive more efficient care with fewer unnecessary tests without duplication of services; and in the end your care will be of better quality. Like motherhood and apple pie – Who could argue with that? Or should we be suspicious? Of course “the devil is in the details.” For instance what is quality care, how do we measure it, and how do we improve it? Medicare has created over twenty “quality care measures” to judge us by and the list (and administrative burden) is growing. There are many ironies here. For instance one Medicare quality measure is to see if we are providing a depression checklist for patients to fill out. Yet if we wish to refer someone to a psychiatrist (good luck finding one), many mental health care providers in our area don’t accept Medicare because the reimbursements are so low and the paperwork too great. Further checklists are for risk of falls and all other manner of things, including seeing if we are in compliance with what are now outdated cholesterol guidelines.
The truth is that Medicare’s struggle to contain costs and improve communication with one’s primary care physician is in part due to our collective glamorization of specialty care. Case in point, we refer you to a cardiologist to make sure your heart is healthy and your tests are thankfully negative. Nonetheless, when you find yourself going back every six months to get your blood pressure checked by their nurse practitioner with yearly expensive tests that don’t change your care, should we be asking Medicare to create an organization to reign in those expensive tests and force the cardiology practice to keep Dr T informed? Might it not be a better choice to have Dr T manage your blood pressure in the first place and let him direct your further care as appropriate?
Repeat that scenario over and over for routine diabetes care, thyroid care, annual prostate checks, etc.; and you can start to see why Medicare finds itself in the position it presently is in: lots of dollars being spent with little to show for it. If nothing else, remember your time is valuable. As a board certified internist surrounded by superb staff, Dr T is well equipped to attend to the majority of your care.
ACOs will likely be with us for a long time to come. We do recommend sharing your health information among all your health care providers. Your participation in the ACO information sharing is voluntary and can be revoked at any time. We are happy to answer any questions about these new and evolving Medicare organizations and how they may impact you.
by Dr Ed Taubman Primary Care Physician Olney MD 301-774-5400
Voted Top Doctor Washingtonian Magazine
Join my Health Blog and get weekly free updates of my health related posts by clicking here
Follow me on twitter @askDrTaubman
Follow me on FB facebook/olneymywellness
Recently Released Data show that new cases of colon cancer and deaths from colon cancer have declined significantly in the past decade. During this period 30% less people have developed colon cancer than in the prior decade. The largest decline has been in those over the age of 65. This coincides with a tripling of the number of seniors undergoing colonoscopy in the same period. Because colon cancers often originate in small non cancerous polyps periodic colonoscopy offers an opportunity to remove polyps before they become cancerous and to find colon cancers at an early stage when they are more easily treated and cured.
Despite these encouraging statistics many people avoid colonoscopy for a variety of reasons. Many people fret over the prep which for the vast majority is no big deal. Others erroneously believe that that since nobody in their family has had colon cancer that they are not at risk. And while it is is true that an important minority of colon cancer has a hereditary basis (listen to Doctor Taubman’s Podcast On the Subject)- the vast majority of patients diagnosed with colon cancer do not have anybody in their family with colon cancer.
While the present data is encouraging two areas of concern are emerging. First, while colon cancer screening usually begins at age 50 (or 10 years before the earliest case in the family), the incidence of colon cancer prior to age 50 appears to be slowly increasing for unclear reasons. Our western diet, sedentary lifestyle and associated weight gain may be contributing. Also colon cancer screening often stops when patients get into their mid seventies though many people nowadays are living a good bit longer. Certainly for those who have never had a colonoscopy and are otherwise healthy a one time colonoscopy at age 75 or beyond is reasonable and supported by the literature.
Colon cancer remains the third most common cancer and cancer related deaths. The progress of the last decade is truly remarkable and a rare example of health care dollars well spent. However 23 million Americans between the ages of 50 and 75 have not been screened for this preventable cancer. Rather than rest on our laurels and celebrating a coalition co-founded by the American Cancer Society and the CDC has set its sights on increasing colon cancer screening from the present reported 55% of those aged 50 to 75 to 80% in the next decade. With colonoscopy becoming more accepted by the population, and insurance coverage becoming more universal that laudable goal should be within reach.
 The CDC and local health departments have begun advising physicians to be on the lookout for cases of an unusual respiratory illness known as MERS. Middle Eastern Respiratory Syndrome was first recognized two years ago, and to date has been thought responsible for about 300 deaths. Initially confined to the Middle East, some cases are beginning to show up worldwide as infected travelers return home. Is this an illness that has been with us for thousands of years and is only now being recognized, or has something basic changed in the causative virus or the way we humans interact with nature? Modern technology is helping researchers to begin to understand what is going on – with many questions yet to be answered. What we do know so far is that the cause of MERS appears to be a virus from the “coronovirus” family of viruses – the same family of viruses that cause the common cold. There is no available vaccine or specific treatment recommended for the virus.
The CDC and local health departments have begun advising physicians to be on the lookout for cases of an unusual respiratory illness known as MERS. Middle Eastern Respiratory Syndrome was first recognized two years ago, and to date has been thought responsible for about 300 deaths. Initially confined to the Middle East, some cases are beginning to show up worldwide as infected travelers return home. Is this an illness that has been with us for thousands of years and is only now being recognized, or has something basic changed in the causative virus or the way we humans interact with nature? Modern technology is helping researchers to begin to understand what is going on – with many questions yet to be answered. What we do know so far is that the cause of MERS appears to be a virus from the “coronovirus” family of viruses – the same family of viruses that cause the common cold. There is no available vaccine or specific treatment recommended for the virus.
According to a recent CDC update all reported cases have originated in the Arabian Peninsula: Egypt, Jordan, Saudi Arabia, Yemen, Oman, UAE, Qatr, Kuwait, Jordan. Initially most of the recognized cases were in severely ill people requiring intensive care and presenting with fever, cough, and shortness of breath. However, just like influenza and many other viruses, there are likely many much milder cases – perhaps just a case of the “sniffles” that affect most people. However, once hospitalized, ill people can spread the virus to health care workers who need to practice meticulous hygiene, including wearing special respirator masks. This is reminiscent of an earlier outbreak of “SARS,” Severe Acute Respiratory Syndrome a different coronovirus imported from China to Canadian health care workers a number of years ago that was eventually controlled by strictly isolating patients and the quarantine of over 5000 people in Toronto alone.
Officials do not know for sure where the MERS virus comes from or exactly how it spreads, but there is increasing evidence that camels may be an important reservoir of the virus. As reported in “Science” magazine, a Dutch team has found that up to 1 in 50 camels in that part of the world carry the virus. In one study 9 percent of those who care for the camels show evidence of having had the virus at some point in the past. The emergence of camel racing as a multi-million dollar sport where camels from over the world are boarded together and age-old customs such as sharing camel milk with guests, and offering camel liver or concentrated virgin camel urine as a delicacy to guests may well play a role in the spread of this virus.
Hopefully the MERS virus outbreak will be contained as was the SARS outbreak in 2002. Those visiting that part of the world should be cautious about drinking camel milk unless pasteurized or eating meat not properly cooked. Those with depressed immune systems with chronic medical conditions such as diabetes, kidney disease, or emphysema should be cautious about being in contact with camels.
At this point anyone who becomes ill with fever and respiratory symptoms after visiting the Arabian Peninsula, or who becomes ill after being around people recently returned from that part of the world, should seek medical care. We have much more to learn about this virus whose recent emergence reminds us that ancient customs, when linked to our modern jet age, can create unique and global medical problems. Fortunately, we also live in an age where we have the technology that so far has been able to to identify and control these outbreaks.
 If you didn’t see it Dr. Oz was called before Congress and chastised for his wild claims that weight loss could magically happen with “fat burning” supplements promoted on his television show. Senator McCaskill took Oz to task for a 2012 show in which he proclaimed that green coffee bean extract was a “magic weight loss cure for every body type.” But Oz did agree that there’s no long-term miracle pill out there without diet and exercise.
If you didn’t see it Dr. Oz was called before Congress and chastised for his wild claims that weight loss could magically happen with “fat burning” supplements promoted on his television show. Senator McCaskill took Oz to task for a 2012 show in which he proclaimed that green coffee bean extract was a “magic weight loss cure for every body type.” But Oz did agree that there’s no long-term miracle pill out there without diet and exercise.
So for once the idea that people can lose weight when given the right nutritional advice and the right tools is getting a look by the public. So where does one go to get the tools he needs to lose weight, without gimmicks, wild supplement claims and scams and have some fun in the process? Where a published nutritionist, doctor, psychotherapist, chef, yoga instructor, and health coach await. Look no further than our own “Olney Integrated Weight Loss Solutions” which we launched in April. Our first group of 25 people lost on average twenty pounds over ten weeks and continue to lose weight. Our next group is forming to start on the week of September 15.
[easychart valuenames=”Week 2, 3, 4, 5, 6, 7, 8, 9, 10, 11,12″ group1values=”1.5,3.0,4.5,6.0,7.5,9.0,10.5,12.0,13.5,15.0,16.5,” group2values=”3.99,8.81,9.09,11.0,13.8,15.4,16.7,17.5,19.5,21.43,23.36″ groupnames=”Goal, Present Group” ]
Program Participants
Author Nutritionist Rick Weissinger RD, MS, CPT
Psychotherapist Andrea Lopes LCSW-C
Yoga Instructor & Personal Trainer Kathi Doan
Washingtonian Top Doctor Edward Taubman, M.D.
Local Chef Debbie Amster Recently Featured On Local TV
This Ten Week Program Meets Weekly From 7:00 to 8:30PM At The Olney Counseling Center at 3430 North High Street
Topics Covered Include
Re-Engineering Your Food Intake – What Should We Be Eating?
Emotional Eating – Identify Your Triggers And Develop Strategies To Manage Them
Get Moving And Relax – Yoga Techniques to Help You Win The Battle
Learn To Cook And Eat Healthy With Cooking Demos
Participation Is Limited To approx 25 people. You can get on the list to attend our next informational meeting on Monday evening September 8 and reserve your Spot for the next group by Filling Out Our Registration Form Below. The present cost is $599 (patients of Dr Edward Taubman and Members of OlneyMyWellness receive a $100 discount).
Call 301-774-5400 for More Information
[si-contact-form form=’5′]
 Many consumers express concerns that aspartame, sucralose, and other artificial sweeteners may not be safe, in spite of their being rigorously researched and approved by scientists and governmental agencies the world over. Below, we will review two of the most commonly used types. We’ll omit saccharin now and in any future discussions, due to the fact that most consumers have replaced saccharin with other non-caloric sweeteners because of its bitter aftertaste.
Many consumers express concerns that aspartame, sucralose, and other artificial sweeteners may not be safe, in spite of their being rigorously researched and approved by scientists and governmental agencies the world over. Below, we will review two of the most commonly used types. We’ll omit saccharin now and in any future discussions, due to the fact that most consumers have replaced saccharin with other non-caloric sweeteners because of its bitter aftertaste.
Sucralose (Splenda): A number of studies with animals suggests both possible side effects and side-benefits for humans. These will not be discussed in detail here, given that they have not been shown to occur in humans as of yet. Briefly however, they involve the possibility of changes in gut hormones that increase satiety and cause insulin secretion, and changes in the number and type of bacteria found in the GI tract.
One possible exception to the lack of data in humans may be of relevance to cancer patients. Sucralose increases the activity of certain proteins that cause the reduced absorption of chemotherapeutic drugs. These proteins are involved in drug resistance, which can complicate cancer treatment. This is not yet thought to be clinically relevant, just a possibility.
Aspartame (Equal, Nutrasweet): As you would expect, all of the studies funded by the industry vouch for its safety, whereas 92% of independently funded studies report that aspartame may cause problems. One of these concerns is the breakdown of aspartame into methanol. This chemical is actually a natural breakdown product of many foods, and a glass of tomato juice provides about 6 times as much methanol as an equivalent amount of diet beverage sweetened with aspartame. Other concerns – including the possibility of cancers, headaches, allergic reactions, and seizures – have, after the publication of carefully designed and controlled studies, not been found to occur.
Those persons who swear that sugar substitutes cause them to experience noxious side effects should stay away from these. It’s well known in the field of mind-body medicine (‘psychobiology’) that, although actual biochemical toxicity may not exist, a reaction may still occur. If a person develops a negative reaction (caused perhaps by food poisoning or new onset of allergy) while having a meal in which a sugar substitute is used, that person will develop a mental association between that sweetener and the reaction. This makes it more likely that the same reaction may be caused by future exposure to that sweetener.
The bottom line is that the preponderance of evidence to date suggests that these substitutes are safe and we have no hesitation in recommending them to patients seeking help to lose weight.
by Ed Taubman M.D. and Rick Weissinger R.D. M.S. Olney, Maryland 301-774-5400
Interested in losing weight? Check out our multidisciplinary weight loss program by clicking here. Our patients are losing an average of 3 pounds a week while eating normal foods and having fun in the process!
The following articles were used as material for this blog post. Readers who want to review these may request the full text versions by E-mail.
Marinovich M et al, Aspartame, low-calorie sweeteners and disease: Regulatory safety and epidemiological issues. Food and Chemical Toxicology 60 (2013) 109–115.
Schiffman SS, Rother KI. Sucralose, A Synthetic Organochlorine Sweetener: Overview of Biological Issues. J Toxicol Environ Health B Crit Rev. Sep 2013; 16(7): 399–451.
Tandel KR. Sugar substitutes: Health controversy over perceived benefits. J Pharmacol Pharmacother. 2011 Oct-Dec; 2(4): 236–243.
 Diet soda is a favorite item among people looking to lose weight or keep weight off. We tend to think of it as a ‘freebie’, calorie-wise, something pleasurable we can enjoy without having to worry about weight gain. Research is conflicting on this topic. There has been increasing suspicion that diet drinks may come with a price, one that may have to be paid in weight gain.
Diet soda is a favorite item among people looking to lose weight or keep weight off. We tend to think of it as a ‘freebie’, calorie-wise, something pleasurable we can enjoy without having to worry about weight gain. Research is conflicting on this topic. There has been increasing suspicion that diet drinks may come with a price, one that may have to be paid in weight gain.
Maybe part of the problem is that some dieters may tend to take advantage (consciously or subconsciously) of the calorie savings with diet drinks. It’s not uncommon to consume roughly the same number of calories with a low fat frozen desert as with regular ice cream, if a larger portion is eaten; similar to a smoker smoking more cigarettes when they are low nicotine. Perhaps some dieters wind up eating more of other foods because they know they’ve saved calories by trading in their regular sodas for calorie free types.
Researchers at the University of Colorado – the same ones who created the National Weight Control Registry and have been involved in obesity research for decades – performed a controlled clinical trial with over 300 people, comparing the effects on weight of drinking diet soda compared with water. In this study, significantly more people in the diet soda group lost 5% of their body weight, compared with people drinking water.
While the results appear to make sense, readers should know that the American Beverage Association sponsored the study. And although a disclaimer states that the ABA had no hand in designing the study or interpreting its results, they clearly benefit from the results.
On the other hand there is some evidence that some people, because their brains are different, may experience an increase in appetite when eating sugar substitutes, while others don’t. And of course, there’s always the possibility that you may ‘train your brain’ to need more sweet-tasting foods by using a lot of sugar substitutes.
So you’re probably wondering – will diet sodas help me in my quest to lose weight? The best strategy for now is to try varying the amounts of these you use, and see if it has an effect on your appetite, hunger, and weight. Next week: Are diet sodas safe?
by Ed Taubman M.D. and Rick Weissinger R.D. M.S. Olney, Maryland 301-774-5400
Interested in losing weight? Check out our multidisciplinary weight loss program by clicking here. Our patients are losing an average of 3 pounds a week while eating normal foods and having fun in the process!
 By Dr. Ed Taubman Olney, Maryland 301-774-5400
By Dr. Ed Taubman Olney, Maryland 301-774-5400
As previously reported by me there continues to be controversy about the idea that those of us who have NOT had a heart attack or stroke should be taking a daily aspirin to prevent one. Bayer recently submitted an application to the FDA to receive permission to promote daily aspirin for this purpose. Many people take a baby aspirin daily because they have heard it is a good thing to do and believe that since it is non prescription must be safe. Many cardiologists recommend daily aspirin to people who have not had a heart attack. Their reasoning is that since aspirin has been shown to benefit people who have had heart attacks or strokes why not give it to healthy people so they don’t develop heart disease or stroke? Similarly since diabetics have a higher risk of heart disease and stroke, endocrinologists often promote daily aspirin to their diabetic patients for the same reasons.
The problem remains, however, that there are no definitive studies that show this to be true. And unfortunately aspirin, though not a prescription drug, can have two very serious side effects. First, it can cause a bleeding ulcer without any warning, which can land people in the hospital with life threatening internal bleeding. Secondly, if a person does get a stroke, those on aspirin are more likely to have a more severe form of stroke known as a hemorrhagic stroke than people not taking aspirin. In fact in 5 studies reviewed by the FDA, 4 studies actually showed an increase in fatal strokes among those taking daily aspirin.
Based on its review the FDA denied Bayer’s request to allow it to promote daily aspirin use for the prevention of heart attack and stroke in those who have never had a heart attack or stroke. For most people the small benefits, if they exist, are probably outweighed by the small but real and potentially serious risks. Nonetheless, there may be a smaller number of patients who are at particularly higher risk for these events and for whom the benefits from daily aspirin outweigh the risks. The challenge is how to identify who those people might be. In future posts we will examine some emerging technologies that propose to do so.
 In case you missed the media hype, recent studies in mice have raised the possibility that someday some of the effects of aging might be reversed. Preliminary research along three tracks in mice suggests that factors found younger blood might have such potential. First researchers joined the circulatory systems of older and younger mice and found that the older mice showed improvements in muscle, heart, liver, spinal cord, and brain tissues. Next, researchers in Boston identified a rejuvenating protein in mouse blood known as growth differentiation factor 11 (GDF11) that may be partially responsible. Recently researchers have found that simply giving older mice transfusions with blood products from younger mice can have a similar effect. So where will all this lead us? Will these concepts work in humans? If it does work, will it be safe or create unanticipated side effects? The field of rejuvenative medicine is in its infancy, so don’t expect fountain of youth treatments any time soon. Normally to take a concept like this, fully understand it, and create a drug that is safe and effective can take a couple of decades. However, since blood products are already given routinely in hospitals for all sorts of reasons, the potential to do trials, say, in Alzheimer’s patients might be considerably sped up. Is it a story that’s too good to be true? Probably, but certainly a story worth following and maybe a classic movie-to-be.
In case you missed the media hype, recent studies in mice have raised the possibility that someday some of the effects of aging might be reversed. Preliminary research along three tracks in mice suggests that factors found younger blood might have such potential. First researchers joined the circulatory systems of older and younger mice and found that the older mice showed improvements in muscle, heart, liver, spinal cord, and brain tissues. Next, researchers in Boston identified a rejuvenating protein in mouse blood known as growth differentiation factor 11 (GDF11) that may be partially responsible. Recently researchers have found that simply giving older mice transfusions with blood products from younger mice can have a similar effect. So where will all this lead us? Will these concepts work in humans? If it does work, will it be safe or create unanticipated side effects? The field of rejuvenative medicine is in its infancy, so don’t expect fountain of youth treatments any time soon. Normally to take a concept like this, fully understand it, and create a drug that is safe and effective can take a couple of decades. However, since blood products are already given routinely in hospitals for all sorts of reasons, the potential to do trials, say, in Alzheimer’s patients might be considerably sped up. Is it a story that’s too good to be true? Probably, but certainly a story worth following and maybe a classic movie-to-be.
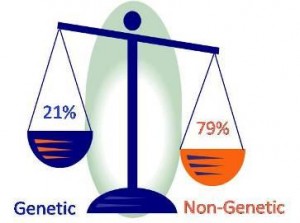 By Dr Ed Taubman, Olney Md 301-774-5400
By Dr Ed Taubman, Olney Md 301-774-5400
With genetic causes of cancer in the general population proving elusive, our focus is increasingly moving towards lifestyle contributions. Increasingly obesity, poor nutrition choices, lack of exercise and alcohol use are being linked to cancer risks. Some experts feel that 1 in 3 cancers in the United States is linked to the above lifestyle issues. Worldwide smoking remains the number one contributor to cancer; but in the United States, as fewer and fewer people smoke and more and more people become overweight, the trend at home has made obesity the number one contributor. And how about alcohol? Alcohol has been declared a carcinogen by the International Association of Research in Cancer. Its breakdown products include 15 known carcinogens from arsenic to formaldehyde. A recent study in the American Journal of Public Health estimated that about 1 in 30 cancer deaths in the United States can be linked to alcohol. Alcohol can raise estrogen levels, and studies have linked three or four drinks a day to increases in breast cancer risk by 40-50%. But surely small amounts of alcohol are okay? Unfortunately, when it comes to cancer, evidence seems to be accumulating that the more one drinks, the greater the risk and that likely there is no amount of alcohol that is safe. Just one drink a day is thought to increase breast cancer risk by about 4%.
So what does the public think about lifestyle change to prevent cancer? In one recently published study 1700 women were asked if they were interested in learning about lifestyle changes to reduce their risk of breast cancer. Of the respondents 41% were interested in learning more about how exercise could reduce their risk, 35% for weight loss, 30% by diet and only 12% were interested in learning about reducing alcohol consumption to cut their risk. Why the disconnect with alcohol? Perhaps it is because alcohol use is so woven into our society as a fun thing to do and its cardiovascular benefits have long been touted. However, for those worried about their cancer risk, lifestyle changes including reducing alcohol consumption to a minimum, becoming more vegetarian, losing weight and exercising seem reasonable and prudent.
 It has been two decades since researchers were able to identify two genes, BRCA1 and then BRCA2. These so-called “breast cancer genes,” when inherited with a faulty copy, would confer very high risks of breast and also ovarian cancers. The thinking was that with time, and as modern genetic tools evolved, researchers would find other genes equally as powerful in causing these and other cancers. Knowing one’s genetic risk might help decide who might need frequent mammograms or MRI’s and who might be able to safely forgo such testing or conversely benefit from preventative measures. Since the discovery of BRCA1 and BRCA2, a few additional high risk breast cancer genes have been discovered such as PALB2, LKB1, and CDH1; but these are very rare. Unfortunately, mother nature has not cooperated with science, and a BRCA3 or BRCA4 has yet to be discovered and may not exist. Instead of a handful of genes that confer great risk, it increasingly looks as if our genetic risk for cancer may be the sum total of hundreds of genes, some of which slightly increase risk, and some of which slightly lower risk.
It has been two decades since researchers were able to identify two genes, BRCA1 and then BRCA2. These so-called “breast cancer genes,” when inherited with a faulty copy, would confer very high risks of breast and also ovarian cancers. The thinking was that with time, and as modern genetic tools evolved, researchers would find other genes equally as powerful in causing these and other cancers. Knowing one’s genetic risk might help decide who might need frequent mammograms or MRI’s and who might be able to safely forgo such testing or conversely benefit from preventative measures. Since the discovery of BRCA1 and BRCA2, a few additional high risk breast cancer genes have been discovered such as PALB2, LKB1, and CDH1; but these are very rare. Unfortunately, mother nature has not cooperated with science, and a BRCA3 or BRCA4 has yet to be discovered and may not exist. Instead of a handful of genes that confer great risk, it increasingly looks as if our genetic risk for cancer may be the sum total of hundreds of genes, some of which slightly increase risk, and some of which slightly lower risk.
Though panels of multiple genes to predict one’s risk are being developed and a few are already commercially available, each of us has over twenty thousand genes and over a million genetic variations are known to occur. So an individual’s risk of developing cancer will likely be a complex and nuanced interplay of subtle genetic variations inherited from one’s mom and dad, which will take a long time to fully understand.
While the scientists are struggling with unraveling our genetic predispositions to cancer, lifestyle issues such as exercise, weight, and alcohol use are increasingly being recognized as contributing as much or more to cancer risk and over which we as individuals have some control. Next week – how interested is the public in reducing cancer risk through lifestyle changes? – Stay tuned for the surprising answer.
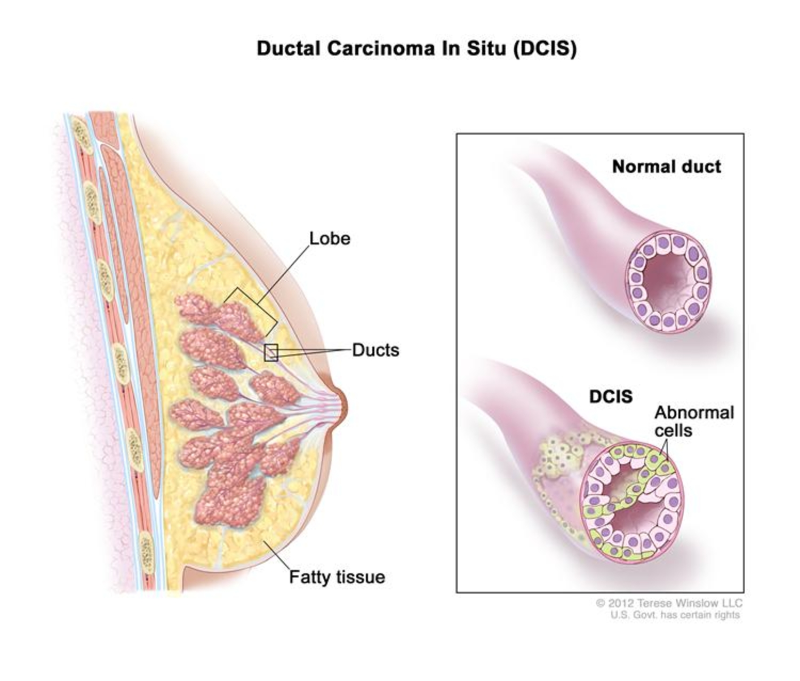 Not all breast cancers are the same. Some start in the part of the breast where milk is manufactured (lobular) and others start in the ducts that carry the milk to the nipple (ductal). Some breast cancers grow very slowly and respond to relatively gentle oral medications, while others are more likely to spread beyond the milk ducts into the surrounding breast or to other parts of the body and require harsh, yet potentially lifesaving chemotherapy. As mammography has over the years become more and more sensitive, a particular kind of breast cancer called ductal carcinoma in situ, or DCIS for short, is being diagnosed much more frequently. These very early cancers are often being diagnosed as tiny specks of calcium on a mammogram that require a magnifying glass to see, and are found so early that, if left untreated, more than half might never cause more serious illness. The challenge is to figure out which women with these very early cancers could forgo radiation, or even surgery, and which are destined to suffer a much more serious problem that needs more aggressive and perhaps life – saving treatment.
Not all breast cancers are the same. Some start in the part of the breast where milk is manufactured (lobular) and others start in the ducts that carry the milk to the nipple (ductal). Some breast cancers grow very slowly and respond to relatively gentle oral medications, while others are more likely to spread beyond the milk ducts into the surrounding breast or to other parts of the body and require harsh, yet potentially lifesaving chemotherapy. As mammography has over the years become more and more sensitive, a particular kind of breast cancer called ductal carcinoma in situ, or DCIS for short, is being diagnosed much more frequently. These very early cancers are often being diagnosed as tiny specks of calcium on a mammogram that require a magnifying glass to see, and are found so early that, if left untreated, more than half might never cause more serious illness. The challenge is to figure out which women with these very early cancers could forgo radiation, or even surgery, and which are destined to suffer a much more serious problem that needs more aggressive and perhaps life – saving treatment.
As outlined in a recent review in “Science” magazine, some researchers are looking at ways to figure out who might really benefit from treatment. Studies are now underway to use new diagnostic tests known as gene array analysis to see who is likely to benefit the most from surgery and radiation and who might just require monitoring. DCIS now accounts for about a third of new breast cancer cases, and by one estimate more than a million women will be diagnosed with DCIS by 2020. In the meantime a healthy lifestyle including eating as little food from animal sources as possible, minimizing alcohol, and getting regular mammograms remain one’s best defense.
And what about the role of genetics? Two decades have passed since the strong breast cancer genetic link between an inherited abnormal BRCA1 or BRCA2 gene was discovered – yet the BRCA genes only account for about 5% of breast cancers. What is the role, if any, of other discovered breast cancer predisposing genes? Next week: Beyond BRCA Gene Testing.
 Studies in the past have showed conflicting results as to the effect of diet on the development of breast cancer. In one of the largest studies reported, over 90,000 pre-menopausal nurses were followed for almost a decade. It was found that the self-reported consumption of red meat and high-fat dairy foods was associated with an increased risk of breast cancer. The authors concluded that animal fat intake was associated with a higher risk of breast cancer; and that by choosing a diet low in red meat and dairy fat, young women would not only be lowering their risk of future heart disease but that they might also lower their risk of breast cancer. To learn more about the role of food in causing and preventing cancer, listen to the podcast between our nutritionist Rick Weissinger and myself on the subject.
Studies in the past have showed conflicting results as to the effect of diet on the development of breast cancer. In one of the largest studies reported, over 90,000 pre-menopausal nurses were followed for almost a decade. It was found that the self-reported consumption of red meat and high-fat dairy foods was associated with an increased risk of breast cancer. The authors concluded that animal fat intake was associated with a higher risk of breast cancer; and that by choosing a diet low in red meat and dairy fat, young women would not only be lowering their risk of future heart disease but that they might also lower their risk of breast cancer. To learn more about the role of food in causing and preventing cancer, listen to the podcast between our nutritionist Rick Weissinger and myself on the subject.
 In recent years Vitamin D, the “sunshine” vitamin, has gone from being important to bone health to a wonder vitamin, said to be capable of stopping all sorts of ailments from cancer to heart disease. As a result a 600 million dollar industry has Americans snatching up vitamin D pills – and some doctors routinely prescribing huge doses – but does it all have any scientific merit?? A recent study in the “Lancet journal of Diabetes and Endocrinology” combined the data of over 30 previous studies and concluded that there was no good evidence that vitamin D supplements actually prevent cancer, stroke, or heart disease. Furthermore, the core belief that vitamin D supplements actually prevent fractures was even called into question. So once again it’s looking like “lifestyle” changes such as staying active, eating lots of vegetables, and exercising remain the most important things one can do to promote health. Want more of that “sunshine” vitamin? You’d be better off getting outside and walking than just popping a pill.
In recent years Vitamin D, the “sunshine” vitamin, has gone from being important to bone health to a wonder vitamin, said to be capable of stopping all sorts of ailments from cancer to heart disease. As a result a 600 million dollar industry has Americans snatching up vitamin D pills – and some doctors routinely prescribing huge doses – but does it all have any scientific merit?? A recent study in the “Lancet journal of Diabetes and Endocrinology” combined the data of over 30 previous studies and concluded that there was no good evidence that vitamin D supplements actually prevent cancer, stroke, or heart disease. Furthermore, the core belief that vitamin D supplements actually prevent fractures was even called into question. So once again it’s looking like “lifestyle” changes such as staying active, eating lots of vegetables, and exercising remain the most important things one can do to promote health. Want more of that “sunshine” vitamin? You’d be better off getting outside and walking than just popping a pill.
 Olney Integrative Weight Loss Solutions Has Launched!
Olney Integrative Weight Loss Solutions Has Launched!
Our participants are steadily losing weight eating regular foods, without supplements or gimmicks, learning how to eat healthy, and having fun in the process.
[easychart valuenames=”Week 2, Week 3, Week 4, Week 5, Week 6, Week 7, Week 8, Week 9, Week 10″ group1values=”1.5,3.0,4.5,6.0,7.5,9.0,10.5,12.0,13.5″ group2values=”3.99,8.81,9.09,11.0,13.8,15.4,16.7,17.5,19.5″ groupnames=”Goal, Present Group” ]
Program Participants
Author Nutritionist Rick Weissinger RD, MS, CPT
Psychotherapist Andrea Lopes LCSW-C
Yoga Instructor & Personal Trainer Kathi Doan
Washingtonian Top Doctor Edward Taubman, M.D.
This Ten Week Program Meets Weekly From 7:00 to 8:30PM At The Olney Counseling Center at 3430 North High Street
Topics Covered Include
Re-Engineering Your Food Intake – What Should We Be Eating?
Emotional Eating – Identify Your Triggers And Develop Strategies To Manage Them
Get Moving And Relax – Yoga Techniques to Help You Win The Battle
Learn To Cook And Eat Healthy With Cooking Demos And Trips To The Grocery Store
At The Olney Counseling Center 3430 N High Street, Olney MD
Participation Is Limited To approx 25 people. Register To Attend Our Next Open House by visiting our new website:
 Recently, articles in the American Annals of Internal Medicine and the British Medical Journal have reviewed the literature and questioned the true role of “saturated fats” in causing heart disease. This of course made a big splash in the media and queries from our patients. We asked our nutritionist Rick Weissinger for his comments below:
Recently, articles in the American Annals of Internal Medicine and the British Medical Journal have reviewed the literature and questioned the true role of “saturated fats” in causing heart disease. This of course made a big splash in the media and queries from our patients. We asked our nutritionist Rick Weissinger for his comments below:
“In these articles, investigators looked at a large number of studies that examined the intake of different fats on the risk for the nation’s #1 killer – heart disease. They thoroughly combed the available studies, including only those of high quality. Based on the health effects of saturated fat on blood cholesterol, the benefits of omega-3’s, and a well-established body of evidence linking unsaturated fats (particularly olive oil) to heart health, the results would have been expected to have concluded: saturated fat BAD; unsaturated fat GOOD.
They didn’t.
The first question is, Why? The Second question: Is it safe to go back to eating cheeseburgers and ice cream again?
There are a number of possible reasons for these results. One is that heart disease has multiple causes, and diet is only one. In addition to the ‘traditional’ risk factors (smoking, family history, high cholesterol), there are about a dozen others, including new emerging risk factors, such as those captured by the VAP blood test done in Dr Taubman’s office. Many of these risk factors are influenced by how much excess weight you’re carrying, how active you are, how stressed you are…and something else not usually considered: the intrauterine environment in which you developed as a fetus.
Forget about all these others for a minute, and let’s focus on aspects of your diet not related to your fat intake. Americans don’t eat anywhere close to the amount of fruit, vegetable, and whole grains recommended by experts. Without these, we don’t get the antioxidants we need to fight atherosclerosis; we don’t get the magnesium we need to prevent our coronary arteries from going into spasm; we don’t get the fiber or chromium we need to keep insulin working normally. And because we don’t eat legumes, we miss out on an important strategy for lowering blood cholesterol which is unequivocally linked to heart disease.
The opinion of this Nutritionist is: we need to look at overall, lifelong dietary patterns if we want to judge whether diet makes a difference in heart disease or not. Studies, which have involved tens of thousands of people from all over the world, have revealed a lower coronary risk in people who eat Mediterranean and traditional (e.g., Asian) diets, and – not surprisingly – a higher risk in people eating a Western diet. Think about that the next time you’re deciding between oatmeal with fruit and a cheese omelet or cheeseburger.”
 We have all heard the phrase “use it or lose it” as it pertains to muscle strength and even mental agility. This had led to a society that values exercise at the gym as much as exercising our brains with crossword puzzles and various mental challenges, in order to slow the aging process. But how does this relate to hearing? Over time, and through the normal course of aging, many of us experience a decline in hearing. This is most often a gradual process that we adapt to, until a loved one begins to complain that the TV is too loud or that they are tired of repeating themselves over and over.
We have all heard the phrase “use it or lose it” as it pertains to muscle strength and even mental agility. This had led to a society that values exercise at the gym as much as exercising our brains with crossword puzzles and various mental challenges, in order to slow the aging process. But how does this relate to hearing? Over time, and through the normal course of aging, many of us experience a decline in hearing. This is most often a gradual process that we adapt to, until a loved one begins to complain that the TV is too loud or that they are tired of repeating themselves over and over.
At this point we are not hearing everything that we should. This is a situation referred to as auditory deprivation. Our hearing relies on nerve endings in our inner ear and complex neural pathways to our brain to interpret the auditory input. When the sound signals are not coming in “loud and clear,” these pathways begin to atrophy and weaken. A number of studies have shown that earlier intervention with hearing aids allows more recovery of these hearing pathways, when compared to those who wait longer and are then never able to fully recover from the period of deprivation.
It is clear that early intervention helps to maintain healthy hearing; and this, in turn, allows us to continue to enjoy the people and activities we love. Seek help as soon as you notice a problem. Encourage you loved ones not to wait. Today’s hearing aids are comfortable, lightweight, very discrete and full of programmable options to customize to your lifestyle. Hearing is one of the joys of life.Don’t neglect it!
by Dr. Heather Schwartzbauer
Heather and her group Montgomery County ENT offer hearing evaluation screening. Call 301-774-0074 to schedule an appointment. Take Our Hearing Health Quiz – Click Here
 A few months back, with the release of the new cholesterol guidelines, we asked the question “Is It Time To Put Statins In the Drinking Water?” Well, now Pfizer, the maker of Lipitor, is trying to move us in that direction by petitioning the FDA to allow an over- the- counter low dose version of Lipitor to be available in pharmacies without a prescription. They have begun a preliminary trial of 1200 consumers who will take a low dose (10mg) of the drug for six months without needing to see a doctor. The study will track whether patients can appropriately comply with instructions to get their cholesterol levels checked in six weeks (they will be able to check using an in- store blood test if needed) and to appropriately consult with a physician if the desired response is not obtained. Proponents suggest that this will give greater access to statins to help reduce heart attack, stroke, and death from heart disease. Others worry that the low dose will end up being used by many consumers who really do not need the medication; and for those who could benefit the most from statins, the 10mg dose will not be nearly high enough. For instance the newer guidelines developed by the American Heart Association and the American College of Cardiology recommend dosing from 40 to 80 mg for those deemed to be at higher risk. It will be interesting to see how all these conflicting points of view are ultimately reconciled by the FDA.
A few months back, with the release of the new cholesterol guidelines, we asked the question “Is It Time To Put Statins In the Drinking Water?” Well, now Pfizer, the maker of Lipitor, is trying to move us in that direction by petitioning the FDA to allow an over- the- counter low dose version of Lipitor to be available in pharmacies without a prescription. They have begun a preliminary trial of 1200 consumers who will take a low dose (10mg) of the drug for six months without needing to see a doctor. The study will track whether patients can appropriately comply with instructions to get their cholesterol levels checked in six weeks (they will be able to check using an in- store blood test if needed) and to appropriately consult with a physician if the desired response is not obtained. Proponents suggest that this will give greater access to statins to help reduce heart attack, stroke, and death from heart disease. Others worry that the low dose will end up being used by many consumers who really do not need the medication; and for those who could benefit the most from statins, the 10mg dose will not be nearly high enough. For instance the newer guidelines developed by the American Heart Association and the American College of Cardiology recommend dosing from 40 to 80 mg for those deemed to be at higher risk. It will be interesting to see how all these conflicting points of view are ultimately reconciled by the FDA.
 Click Here To Take Our Skin Health Quiz And Learn More About Keeping Your Skin Healthy
Click Here To Take Our Skin Health Quiz And Learn More About Keeping Your Skin Healthy
New, OlneyMyWellness Members Get A FREE Refresher Facial at Serenity Zone Medical Spa on their Birthday – a $60 value (you must present Birthday E-mail from OlneyMyWellness)
 When I see otherwise healthy patients in the office and review their medications, I often find that they are taking a daily aspirin. When I ask them why, I often get a puzzled look. When I ask who suggested that they do so, they often say, “Well, nobody. I just heard it was a good thing to do.” So is it true? Actually, there recently has been a flurry of articles on the subject.
When I see otherwise healthy patients in the office and review their medications, I often find that they are taking a daily aspirin. When I ask them why, I often get a puzzled look. When I ask who suggested that they do so, they often say, “Well, nobody. I just heard it was a good thing to do.” So is it true? Actually, there recently has been a flurry of articles on the subject.
For starters taking a daily aspirin has been heavily promoted as a way to prevent heart attacks, strokes, and even cancer. However, a recent review of over a hundred studies shows minimal, if any, such benefits in otherwise healthy people. What about harms? Even though aspirin is available without a prescription, it still is a drug; and, like any drug, it can have serious side effects as well as adverse interactions with other medications. For instance it can decrease the effectiveness of certain blood pressure medications.
The most serious side effect is bleeding of the stomach and intestines which can begin suddenly and without any prior warning. Such bleeding can be life-threatening and require emergent hospitalization, blood transfusions, and need for emergency procedures or even surgery. The anti-clotting effects of aspirin can also lead to bleeding in other parts of the body such as the brain. Concerned about your hearing? Aspirin use has been linked to loss of hearing. Concerned about your eyesight? Aspirin use has been linked to progression of macular degeneration.
So who should take a daily aspirin? People who have known heart problems such as atrial fibrillation and who are not already taking more effective blood thinners such as coumadin, pradaxa, xarelto and others; and people who have vascular stents, who are exhibiting stroke symptoms such as TIAs and or who have otherwise been so directed by their physicians. In those cases the benefits may outweigh the risks. However, for the rest of us, its daily use remains unproven and has the potential to do more harm than good.
 There are many arguments to make in regards to the benefits accrued by insuring more Americans. One of the anticipated benefits is to decrease the use of emergency room services by the uninsured, who often do not have a primary care physician. A recent study published in ” Science” magazine by Taubman (no relation) and others studied the effect of expanded government – sponsored health insurance in Oregon on emergency room usage. What they found was just the opposite. Newly insured patients used the emergency room 40% more than their uninsured counterparts. The increase in visits was across a broad range of conditions, and the vast majority of the increased visits could have been treated in lower cost primary care physician offices. An accompanying editorial states, “It is possible to argue that this represents greater access to necessary care, or that it shows that insurance serves as further encouragement to seek unnecessarily expensive treatment……Based on this paper’s findings, we have a good reason to anticipate a large increase – and almost surely not a decrease – in traffic to already overburdened emergency departments across the country.”
There are many arguments to make in regards to the benefits accrued by insuring more Americans. One of the anticipated benefits is to decrease the use of emergency room services by the uninsured, who often do not have a primary care physician. A recent study published in ” Science” magazine by Taubman (no relation) and others studied the effect of expanded government – sponsored health insurance in Oregon on emergency room usage. What they found was just the opposite. Newly insured patients used the emergency room 40% more than their uninsured counterparts. The increase in visits was across a broad range of conditions, and the vast majority of the increased visits could have been treated in lower cost primary care physician offices. An accompanying editorial states, “It is possible to argue that this represents greater access to necessary care, or that it shows that insurance serves as further encouragement to seek unnecessarily expensive treatment……Based on this paper’s findings, we have a good reason to anticipate a large increase – and almost surely not a decrease – in traffic to already overburdened emergency departments across the country.”
The reasons for the observed increases in ER use are likely many. One reason may be that patients are just doing what they were told; many busy primary care practices who already have schedules filled with non-emergent cases may tell patients to go to the emergency room so as not to disrupt their schedules. In addition more and more primary care practices employ physician extenders such as nurse practitioners and physician assistants who do not have the training or experience that allows them to comfortably see and treat sicker patients in an office setting. By contrast, in our unique practice model we always keep slots open for sick visits and whenever possible attend to people the same day. Finally, many hospitals (for profit and non- profit) incessantly advertise that patients should come and utilize their emergency rooms by instilling fear that a routine flu might be something more serious. While this may be good for the hospital’s bottom line, that calculus may be changing in Maryland (see previous post on Maryland Medicare Waiver).
Regardless of the causes, the health care system has to deal with the consequences. Warns the editorial, “Whether or not you think universal coverage is a good idea, we had better start planning for it.”
 Results of the New Dietary Interventions to Enhance the Treatments for Weight Loss (NewDIETs) Study
Results of the New Dietary Interventions to Enhance the Treatments for Weight Loss (NewDIETs) Study
ATLANTA, GA – Most weight-loss interventions focus on reducing calories, but a new study shows that vegan and vegetarian dietary patterns can result in more weight loss than those that include meat without emphasizing caloric restriction. Results of the study were presented at a special session of The Obesity Society Annual Meeting.
“Many researchers agree that vegan eating styles are tied to lower BMI, lower prevalence of type 2 diabetes, and less weight gain with age,” said lead researcher Brie Turner-McGrievy, PhD, of the University of South Carolina. “We found that participants consuming vegan and vegetarian diets lost an average of 8.2 to 9.9 pounds over eight weeks while those consuming some meat lost 5.1 pounds.” At 6 months the vegans had lost 7% of their body weight, and those consuming meat 3%.
The reason for greater weight loss in the vegan and vegetarian groups remains to be studied, but may be due to changes in macronutrient content. In addition participants in this study most likely ate fewer calories as a result of the dietary changes they made to consume more vegan or vegetarian meals.
Said author Dr. Turner-McGrievy, “Diets that focus primarily on calorie restriction are a cornerstone of weight loss programs; however, they usually involve dietary self-monitoring, which many individuals find burdensome and can limit adherence.”
Because weight loss achieved by patients following plant-based diets in this study occurred without emphasizing caloric restriction, some individuals may find these types of dietary patterns easier to follow over the long term, according to the researchers.
This study validates many of the principles incorporated into the weight loss program run by our own nutritionist, Rick Weissinger R.D. M.S. Our program includes experts in yoga, exercise, psychotherapy, and even includes cooking lessons by a local chef. To learn more about our multidisciplinary weight loss program and how to get on our waiting list for our next informational open house, click here
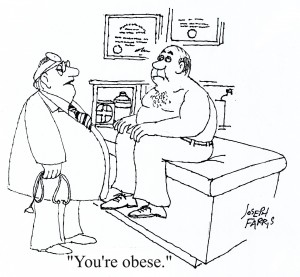 According to the CDC an estimated 97 million adults in the United States are overweight or obese, a condition that substantially raises their risk of hypertension, high cholesterol, diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea and respiratory problems, and cancers of the breast, prostate, and colon. CDC data show that about a third of adults are overweight, an additional 36% are obese, and 6% are classified as extremely obese.
According to the CDC an estimated 97 million adults in the United States are overweight or obese, a condition that substantially raises their risk of hypertension, high cholesterol, diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea and respiratory problems, and cancers of the breast, prostate, and colon. CDC data show that about a third of adults are overweight, an additional 36% are obese, and 6% are classified as extremely obese.
Do physicians practice what they preach when it comes to diet, nutrition, and maintaining a healthy weight? In a recently published study the percentage of physicians who are overweight were compared by specialty. The surgeons topped the scales – is it because they spend a lot of time standing and don’t have time to plan meals? The dermatologists and plastic surgeons were lightweights – maybe they are more self conscious of the image they need to project. And what about those gastroenterologists……
Overweight is defined as a BMI (Body Mass Index) between 25 and 30. Obesity is a BMI of 30 or more, though some think the number should be 27 or 28 as that’s when significant adverse health consequences start to kick in. Curious how you compare? Click here to calculate your BMI
Losing weight and then keeping it off can be difficult. Need help? – We’ve put together our own multidisciplinary program Click Here For Details
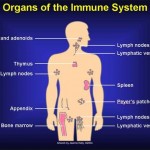 A role of our immune system in preventing cancer has been postulated for over 50 years. However, it has only been recently that researchers have been able to begin to unravel the complexity of the immune system’s role in cancer and begin to harness the immune system to fight cancer.
A role of our immune system in preventing cancer has been postulated for over 50 years. However, it has only been recently that researchers have been able to begin to unravel the complexity of the immune system’s role in cancer and begin to harness the immune system to fight cancer.
Present research suggests that from time to time we may all be developing cancerous cells which are kept in check by our immune systems. One of the mysteries of advanced cancer has been why some cancerous cells are able to escape from immune suppression so that the immune system does not always effectively attack one’s cancer. Under the microscope cancer-fighting T-lymphocytes can be seen surrounding cancer cells but not killing them. One reason that has been discovered is that some cancers may produce signals that tell the “T” cells to go into a kind of immune hibernation. Newly developed drugs block these cancer produced signals and, in certain cancers, have led to dramatic cancer shrinkage.
Normally T cells have a limited life span and die via a normal phenomena known as apoptosis. A new class of drugs called “programmed death” or PD-1 inhibitors tells T cells to stick around longer and not die so that they can more effectively fight cancers. In yet another strategy, pioneered locally at the National Cancer Institute, T cells are removed from tumors, genetically re-engineered to make them better cancer fighters, and then re-infused back into the patient. The advantage of this type of therapy is that the new T cells can take up residence in the body and be around for a long time to perpetually keep the cancer on the run.
Researchers are working on combinations of these different strategies and trying to figure out how to prevent unintended serious side effects, such as the activated and aggressive cancer fighting T cells not attacking normal tissues. Some of these strategies require individualizing treatments for each cancer, and each individual, and thus are not presently practical on a large scale. The field is in its infancy but nonetheless has been making dramatic progress. In our own practice we have seen a few patients begin to benefit from these new therapies. Many of the researchers have been working on this for their entire careers. They, and the institutions that have supported them, deserve a lot of thanks for their efforts that hopefully will eventually lead to a new era in cancer treatment.
 On January 10, 2014, the Centers for Medicare & Medicaid Services (CMS) and the state of Maryland jointly announced a new initiative to “modernize Maryland’s unique All-Payor rate-setting system for hospital services that will improve patient health and reduce costs.” Sounds great, “improve patient health and reduce costs,” but what is the reality? Well, first one has to understand the uniqueness of the present system in Maryland.
On January 10, 2014, the Centers for Medicare & Medicaid Services (CMS) and the state of Maryland jointly announced a new initiative to “modernize Maryland’s unique All-Payor rate-setting system for hospital services that will improve patient health and reduce costs.” Sounds great, “improve patient health and reduce costs,” but what is the reality? Well, first one has to understand the uniqueness of the present system in Maryland.
Four decades ago the state was faced with a number of disturbing trends. Hospital costs in Maryland were rising much faster than the national average and Maryland hospitals with high levels of uninsured patients were on the verge of bankruptcy. In other states, such as California, hospitals were said to be engaged in rampant “cost shifting” and “patient dumping” whereby patients without insurance were being refused by profitable hospitals. Around this time Medicare was starting to come up with its own solutions.
Not wanting to cede control to the emerging payment policies of the federal government, the state developed its own unique “All-Payor” hospital system and convinced the federal government to issue Maryland a waiver from the Medicare payment system. To keep hospital costs from exploding, a Hospital Services Cost Review Commission was created; and all insurance companies were required to pay hospitals the same rate mandated by the commission rather than negotiated by the individual hospitals and insurance companies. The rates paid could differ from hospital to hospital, depending on its mix of uninsured. From a social policy point of view, the program was successful. It kept hospitals solvent, provided a dependable method for hospitals to get paid, and obviated the need for public hospitals for the uninsured.
For 36 years Maryland remained the only state in the union to have been granted and kept its Medicare exemption. However, as health care evolved, the Maryland system did not. With health care shifting increasingly to an outpatient setting, the inpatient Maryland model no longer was capable of keeping global health costs down for a number of reasons, many self-inflicted.
State agencies allowed large hospital conglomerates such as Medstar to take over multiple smaller hospitals and then get into the business of running outpatient services while charging and getting paid higher inpatient rates. Meanwhile, the Cost Review Commission continued to approve costly additions to hospitals offering duplicate services even as hospital occupancy rates were falling. Finally, insurance companies such as United (annual profits of over $5 billion) were allowed to maximize their profits in the face of increasing hospital costs by cutting reimbursements to experienced primary care practices to 20% or less than Medicare. Add to that the debacle of the Maryland Health Exchange, the premise that the exchange would foster competition among health insurers was laid bare when Cigna and Aetna could not be convinced or cajoled to participate, essentially leaving just United, Carefirst, and Kaiser to participate.
To keep its cherished waiver Maryland has agreed to require Maryland hospitals to keep annual increases for both inpatient and outpatient services not to exceed 3.58% over the next five years and thereby generate $330 million in Medicare savings over a five-year performance period. Also the hospitals will need to initiate programs to improve their quality ratings. In theory, if Maryland can’t pull this off, they will then lose the waiver (unless the politicians get involved as they likely did this time around).
So where does that leave us? At the end of the day, we are left with a system in Maryland essentially dominated by a couple of monolithic health care companies (United and Carefirst) with little competition, huge hospital systems which for years have gotten used to being fed a rich diet doled out by order of the state, and a decimated primary care system.
The likely scenario will be an acceleration of present trends, more consolidation and less competition, doctors with years of training and experience replaced by mid levels (nurse practitioners and physician assistants just graduated from college), registered nurses with years of training replaced by medical assistants with weeks of training, quality assessed by bureaucratic checklists, and cost savings to pay for all those new shiny buildings coming from layoffs of the most important asset – experienced people.
 Some of our patients have asked about taking Biotin to treat hair loss and brittle nails. I asked our nutritionist Rick to comment:
Some of our patients have asked about taking Biotin to treat hair loss and brittle nails. I asked our nutritionist Rick to comment:
Biotin deficiency causes structural changes in the hair and nails. However, biotin deficiency is rare, because your gut bacteria actually make it. The people most likely to suffer from biotin deficiency include: those taking antibiotics for long periods of time; people eating raw egg white; and possibly anti-seizure medications. There’s no evidence that people with hair loss or changes in hair quality have benefited from biotin supplements. Nails may be another story. Human studies found that the overwhelming majority of women with brittle fingernails who took biotin (2.5 milligrams of biotin each day for up to 6 months) saw improvements in nail quality (i.e., less splitting and cracking). However, none of these were ‘controlled’ trials, so the jury is still out.
Good food sources include whole wheat bread, avocado, raspberries, and cauliflower.
Rick Weissinger, MS, RD, LDN, CPT
Author, WHAT THE EXPERTS SAY ABOUT FOOD AND CANCER
Co-author, NUTRITION GUIDE FOR CLINICIANS, editions 1 and 2
Web site: www.idomnt.com
Phone: (301) 525-9078
 May You Finally Get That Colonoscopy That You Have Been Putting Off
May You Finally Get That Colonoscopy That You Have Been Putting Off
May Your Donut Hole and Waist Lines Be Shrinking
May Your HDLs All Be High and Your LDLs Low
May Your Exercise Be Increasing And Your Diet Becoming More Vegan
May You Finally Get That Sleep Study Before Your Snoring Shakes Down The House
May You Finally Get That Shingles Shot Even If Medicare Won’t Pay
May Obamacare Be Kind To You And High Deductibles Stay Away
Best Wishes For A Happy And Healthy New Year From Dr Taubman & Staff
 FDA…“More than 5 years after you began marketing, you still had not completed some of the studies and had not even started other studies necessary to support a marketing submission for the PGS (Personalized Genomic Services)…. We still do not have any assurance that the firm has analytically or clinically validated the PGS for its intended uses…. The company is therefore barred from sales of the service for any potential medical applications until the necessary data is submitted and a regulatory decision made.” Click Here For Part 1
FDA…“More than 5 years after you began marketing, you still had not completed some of the studies and had not even started other studies necessary to support a marketing submission for the PGS (Personalized Genomic Services)…. We still do not have any assurance that the firm has analytically or clinically validated the PGS for its intended uses…. The company is therefore barred from sales of the service for any potential medical applications until the necessary data is submitted and a regulatory decision made.” Click Here For Part 1
23andMe On Its Website… “At this time, we have suspended our health-related genetic tests to comply with the U.S. Food and Drug Administration’s directive to discontinue new consumer access during our regulatory review process. In the future, you may be able to receive health-related results, dependent upon FDA marketing authorization.”
So where did 23andMe, a company whose product in 2008 was named by “Time” as the Invention of the Year, go wrong?
Certainly a big part of it is that the premise in 2007 that analyzing more and more genetic variations would make it obvious to all what our medical destiny would be has not really turned out to be the case for common ailments like heart disease, diabetes, and cancer. At a technical level the 23andMe model relies heavily on what in the trade is called Genome Wide Associations. Such associations tend to be weak and complicated by the unknowns of how multiple variations, some implying higher risk, some lower, and the environment all interact. And, assuming that the numbers they quote were actually accurate, which is questionable and to which the FDA is demanding proof, does knowing that your risk of prostate cancer is 10% greater than the average really help you? Probably not. Rather, such weak associations have been most helpful to researchers looking for tea leave signs of what causes cancers and other ailments and to develop medicines to treat them.
Now, it is true that a handful of genetic variations have been strongly linked to a significant risk of cancer in an important minority of people. BRCA testing for risk of ovarian/breast cancer and Lynch Syndrome testing for hereditary colon cancers are the two most important examples where genetic testing can be helpful and even life-saving. Unfortunately, this is where 23andMe really in my opinion dropped the ball and the FDA really pounced on the BRCA example. The fact is BRCA testing really does require a trained professional to explain, yet 23andMe does not offer access to genetic counseling – just your results. And as a primary care physician who spent three months in training from the City of Hope in these matters, and who gets referrals from other primary care doctors, oncologists and other specialists to spend over an hour explaining the pros and cons of being tested, the ins and outs of what a negative result, a deleterious result, and a variant of unknown significance truly mean – What 23andMe offered in this regard was glaringly incomplete and potentially ripe for misunderstanding by some patients and even some doctors.
For instance there are hundreds of genetic variations that are cancer predisposing within the BRCA genes, but only three were being checked for and reported by 23andMe; plus the methodology they used to test for those three while Myriad held the patent was not transparent. Furthermore, the genetics of BRCA – associated breast and ovarian cancers can get complicated. For instance, it is now well known that wholesale missing parts of BRCA genes, or the opposite, duplications, are not easily captured by the testing 23andMe performs, yet can create the same high disease risk. Checking for these duplications and deletions requires a different technology than that offered on the chip that 23andMe uses.
At the end of the day, their business model and philosophy that “it’s your DNA and you should have access to it” minimalized the concept that this can be complicated stuff that should involve medical professionals. In a telling interview in the “New York Times” in 2010, which in retrospect they might now regret, Esther Dyson, a director of 23andMe was quoted as saying it is “appallingly paternalistic, to think consumers could not interpret genetic information without help of a doctor… People can understand statistics about baseball,” she said, “and I think they ought to understand statistics about genetics.”
Obviously, the FDA disagreed. What do you think?? [polldaddy poll=7679176]
p.s. like what you are reading? Please share with your friends and neighbors using the links below! Want to start a new topic or start receiving weekly e-mail summaries of our health blog? Click Here
 The first new national blood pressure guidelines in over ten years are out, and I think it fair to say that they say as much about how medicine is to be practiced in the future as they do about the treatment of blood pressure. First about the recommendations themselves:
The first new national blood pressure guidelines in over ten years are out, and I think it fair to say that they say as much about how medicine is to be practiced in the future as they do about the treatment of blood pressure. First about the recommendations themselves:
On the heels of the recent changes in cholesterol guidelines, it is fair to question the whole process of how these sweeping recommendations get made and where the process is taking us.
Both the cholesterol guidelines group and the hypertension guidelines group were appointed by the National Heart, Lung, and Blood Institute of the NIH. That is where the similarities tend to end. For example:
The cholesterol group tried to take a holistic approach to help decide who would benefit from statins by coming up with a formula that took into account other risk factors, such as the presence of diabetes, hypertension, smoking history, age, sex, and ethnicity. The hypertension group only took into account age. As patients with high cholesterol often have hypertension, it is difficult to reconcile these different approaches.
The cholesterol group looked for answers by reviewing different kind of studies, sometimes using studies of the “meta-analysis” – and “observational” type. The hypertension group instead looked almost exclusively at types of studies known as “randomized controlled trials”. Randomized controlled studies on large groups of people are very expensive to do so there are not that many out there to review.
In the absence of studies to prove something true, the cholesterol group was more likely to use a consensus of experts to come up with recommendations; while for the hypertension group, the absence of hard proof often meant no recommendation or even retraction of a previous recommendation. The case of blood pressure targets in diabetics is an example: For years primary care physicians, diabetic specialists, cardiologists, eye specialists, and kidney doctors have been advocating making the blood pressure goal for diabetics lower than for the average person in the hope that this would forestall some of the feared complications of the diabetes. However, the hypertension group felt there were no definitive studies out there to answer the question as to whether that really was true and therefore deemed the lower blood pressure goal no longer valid. According to this type of thinking, no definitive data one way or the other carries the same weight as adverse data.
Depending on one’s personal experience and training, different doctors may agree or disagree with some of these newer guidelines. I for one have always advocated less strict guidelines for elderly patients in the treatment of hypertension because of concerns about falls caused by over treatment, but conversely feel that most diabetics should strive for a lower blood pressure goal than the average person.
To be sure coming up with recommendations can be difficult. Definitive answers are not easy to come by particularly when a treatment may take decades to show an effect, as is the case with arteriosclerosis. Think of the new house you bought thirty years ago; now a pipe develops a leak. Was the leak due to the fact that the pipe was a then new plastic, or that ten years ago you switched from well to city water, or maybe it was that water heater that had a recall? Can’t figure out the reason for the leak? How about looking at the leak experiences of ten thousand homeowners combined? Still can’t find the answer? How about looking at the collective experience of a million homeowners? Aha! You think you’ve found the cause – but did you? Because now those million homeowners are spread out over different states with varying temperatures and humidity. Well, you get the picture.
Yet, when you see how different groups of smart people can come up with such seemingly divergent approaches to analyzing the literature and making recommendations, you can’t help but wonder if what we are seeing here has as much to do with who is invited to be on these groups and the personalities of group members and their leaders. For those of you who have served on committees given expansive charges and latitude, this should be no surprise.
These “recommendations” are becoming increasingly important for a number of reasons. First, for those interested in promoting quality they provide a quick and easy way to judge the “quality of care”. So, if all your patients are meeting the new guidelines then your care is considered good – Never mind that last year when the guideline recommendations were different your care was considered less than optimal. Insurance companies such as United Health (profits of 7.2 billion dollars last year) want to prove to their large group customers that there is value to the high premiums they charge and that they are doing something to help keep their employees healthy. As a result tracking adherence to recommendations has itself become a big business as insurance companies contract with companies to scan medical records and review prescription records and then send faxes to doctor’s offices suggesting changes in medications. What we really need is a study to see if any of this accomplishes anything other than killing a lot of trees and diverting doctors and their staff from doing what they are supposed to do – which is to take care of you.
Similarly, in the name of “quality” insurance companies may not want to pay for medications for individuals who are outside the “recommendations” unless the doctor’s office goes through a complicated prior authorization process. Finally, these one size fit all recommendations fit well into a growing pattern whereby experienced physicians are being judged by computerized checklists and increasingly replaced by non physicians such as nurse practitioners and physician assistants who, given their more limited experience and training, are more likely to use computer generated guidelines when providing care and less likely to step outside the box.
There was a time when patients came to their physician with the hope that their doctor’s experience would help them come up with a recommendation personalized to them. In the medical field we call that “clinical judgment”. And the sign of a doctor with good clinical judgment was that, when they didn’t know the answer, they would ask a colleague whom they trusted to share their expertise. Medical reports then tended to read, “In my experience Mary would benefit by….” Nowadays the computerized reports tend to read, “According to the Jupiter trial Mary would benefit by…” For better or worse – the new recommendations, and in particular those of the hypertension group, seem to be taking us further away from that lofty goal of personalized medicine.
p.s. Like what you are reading? Please share with your friends and neighbors using the links below! Want to start a new topic or start receiving weekly e-mail summaries of our health blog?? Click Here
 The year is 2007 and the genetic revolution is in full swing. Medical science has already performed the initial sequencing of the human genome at a cost of a few billion dollars for the first dozen or so people tested and now the cost of genetic testing is dropping from hundreds of millions of dollars per individual to hundreds of thousands to ten thousand dollars and the idea takes hold that we would soon each have affordable access to our personal genome. Empowered by the knowledge of what illnesses we would be destined to get we could be proactive. Worried about diabetes risk? Just check your DNA and if not predisposed eat what you want to. Worried about heart disease? – well maybe there are screenings that you need to start undergoing earlier in life than the average person – Or perhaps your risk is actually genetically so low so you don’t need to take statins or blood pressure medications and can avoid the costs and side effects that your neighbors have to put up with. And for those who don’t like going to the doctor why not order the test yourself and have the results delivered privately via e-mail? Enter a company called 23andMe which set out to do just that. The premise was both simple and yet daunting. Just categorize the genetic differences among us, link them to certain disease risks, and disseminate the information. No need for doctors, or genetic counselors. It’s your DNA after all and you should have complete access to it.
The year is 2007 and the genetic revolution is in full swing. Medical science has already performed the initial sequencing of the human genome at a cost of a few billion dollars for the first dozen or so people tested and now the cost of genetic testing is dropping from hundreds of millions of dollars per individual to hundreds of thousands to ten thousand dollars and the idea takes hold that we would soon each have affordable access to our personal genome. Empowered by the knowledge of what illnesses we would be destined to get we could be proactive. Worried about diabetes risk? Just check your DNA and if not predisposed eat what you want to. Worried about heart disease? – well maybe there are screenings that you need to start undergoing earlier in life than the average person – Or perhaps your risk is actually genetically so low so you don’t need to take statins or blood pressure medications and can avoid the costs and side effects that your neighbors have to put up with. And for those who don’t like going to the doctor why not order the test yourself and have the results delivered privately via e-mail? Enter a company called 23andMe which set out to do just that. The premise was both simple and yet daunting. Just categorize the genetic differences among us, link them to certain disease risks, and disseminate the information. No need for doctors, or genetic counselors. It’s your DNA after all and you should have complete access to it.
The logistics of doing this were significant. Our DNA contains 3 billion bits of information called bases. This instruction set for life is surprisingly identical for each of us – most of that information is mission critical and has been preserved unchanged over hundreds of millions of years – yet there is some variation that is allowed by mother nature. On average one in a thousand or so bases can be different. A simple calculation shows there potentially to be over a million differences among us! Those differences help shape who we are and potentially our disease risks.
Genetic companies like 23andMe use chips that can test for an increasing number of these variations. Like buying a camera with more and more pixels for less and less money the cost and power of the chips to analyze our genetic data has continued to fall with more and more of those million plus variants coming into focus with each new generation of chip.
How to manage and make statistical significance of all this information? 23andMe teamed up with google who provided money and use of their powerful computers to analyze the massive amounts of data.
With the falling price of chips 23andMe began offering testing for less than $100 and upped their marketing campaign for their saliva based home DNA personalized genome testing. However, this year instead of a DNA collection kit in your Xmas stocking, as 23andMe had hoped, they instead got a bit of coal with an FDA warning now on their website which says “At this time, we have suspended our health-related genetic tests to comply with the U.S. Food and Drug Administration’s directive to discontinue new consumer access during our regulatory review process. In the future, you may be able to receive health-related results, dependent upon FDA marketing authorization.”
So what went wrong and why did the FDA (sometimes called the Foot Dragging Administration by its critics) step in? Click Here for part 2.
p.s. like what you are reading? Please share with your friends and neighbors using the links below! Want to start a new topic? Click Here
 The importance of core strength can’t be overstated. However, with soo much misinformation, fad diets and exercises out there, it can be confusing as to what core training is truly about.
The importance of core strength can’t be overstated. However, with soo much misinformation, fad diets and exercises out there, it can be confusing as to what core training is truly about.
The core is much more than just the abdominal or “six pack” muscles. It is actually a collection of muscles that’s main purpose is to stabilize the spine. The spine is essentially the chassis of the body. It is responsible for transmitting forces from the lower extremities and upper extremities. If there is weakness in the core musculature, compensations and movement dysfunctions and injuries can arise. Luckily, there are many ways to safely and effectively train the core, no matter what your current fitness level is.
Below is a great video featuring Professor Stuart McGill speaking about the spine, and the core musculature’s role in keeping it safe and secure.
If you have any questions about strengthening your core, or any questions regarding fitness, mobility/flexibility- please feel free to contact me at:
justinmccary@gmail.com
Hope this was beneficial. Enjoy!
– Justin
 Like what you are reading? We would appreciate your going to our facebook page www.facebook.com/olneymywellness liking the page, the posts, and writing a review. Thx
Like what you are reading? We would appreciate your going to our facebook page www.facebook.com/olneymywellness liking the page, the posts, and writing a review. Thx
 Coincident with recently released guidelines recommending increased use of statins to reduce heart attacks, stroke, and sudden death there is renewed interest in the safety of the statin class of medications. Do they for instance increase or for that matter decrease one’s risk of cancer? When the first statin Mevacor was released three decades ago there was concern about studies in rodents showing increased tumors. However, as the years have gone by there have been many studies suggesting that statins actually decrease cancers such as colon and prostate. Recently there were two studies that received news media attention that seemingly reached opposite conclusions. One from the Fred Hutchinson Cancer Center in Seattle suggesting that women taking statins for over 10 years had a higher risk of breast cancer. Conversely, a study by researchers at Duke using mice suggests that cholesterol may play a pivotal role in causing aggressive breast cancers and that statins might be useful in treating or preventing such cancers. The bottom line is that cancer is complex and after thirty years of statin use in people we really don’t have an answer one way or the other.
Coincident with recently released guidelines recommending increased use of statins to reduce heart attacks, stroke, and sudden death there is renewed interest in the safety of the statin class of medications. Do they for instance increase or for that matter decrease one’s risk of cancer? When the first statin Mevacor was released three decades ago there was concern about studies in rodents showing increased tumors. However, as the years have gone by there have been many studies suggesting that statins actually decrease cancers such as colon and prostate. Recently there were two studies that received news media attention that seemingly reached opposite conclusions. One from the Fred Hutchinson Cancer Center in Seattle suggesting that women taking statins for over 10 years had a higher risk of breast cancer. Conversely, a study by researchers at Duke using mice suggests that cholesterol may play a pivotal role in causing aggressive breast cancers and that statins might be useful in treating or preventing such cancers. The bottom line is that cancer is complex and after thirty years of statin use in people we really don’t have an answer one way or the other.
 Does Breast Cancer Seem to Run in Your Family? Take our Hereditary Breast Cancer Quiz and Learn More
Does Breast Cancer Seem to Run in Your Family? Take our Hereditary Breast Cancer Quiz and Learn More
 The recent joint recommendations of the American College of Cardiology, the NIH, and the American Heart Association has generated a number of controversies particularly about the expanded role for the statin class of medications in lowering the risk of heart attack, stroke, and sudden death. Some of the controversies include:
The recent joint recommendations of the American College of Cardiology, the NIH, and the American Heart Association has generated a number of controversies particularly about the expanded role for the statin class of medications in lowering the risk of heart attack, stroke, and sudden death. Some of the controversies include:
In regards to statins causing diabetes the joint working group reviewed a number of articles that suggested that there is some preliminary evidence that statins might for unknown reasons increase a person’s risk of developing diabetes. So what might that risk be? The group cited a preliminary statistic of .1 to .3 new cases of diabetes per year for every 100 people taking the medication. The lower number was for weaker statins and the higher number for more potent ones. So to simplify, let’s use a number of .2 If 100 people took statin for ten years then there might be 2 more cases of diabetes than might otherwise have been expected and similarly if 100 people took statins for twenty years there might be an additional 4 cases of diabetes than would otherwise have been expected. Put another way – if twenty years ago a 50 year old was started on statins then today at age 70 by my calculation he or she might incur a 4% additional risk of having diabetes than would otherwise have been expected. To keep that in perspective the CDC in its 2011 National Diabetes Fact Sheet stated that almost 27% of Americans over the age of 65 presently have diabetes. What is not clear is if diabetes that may develop on statins will cause the same degree of diabetic complications as non statin related diabetes. One could argue that since statins clearly reduce cardiovascular complications in people who are already diabetics that those who develop diabetes while on statins might be expected to have less complications. In fact the working group recommended that all diabetes be on statins, regardless of their cholesterol levels. After reviewing all the presently available data the working group felt that at least when it comes to concerns about diabetes that the pros of statins greatly outweighed the potential cons. Clearly the researchers will be closely watching this issue in the years to come. What do you think?
Next week statins and cancer.
 Its time to reflect and I give Thanks for being blessed with such a wonderful family and staff:
Its time to reflect and I give Thanks for being blessed with such a wonderful family and staff:
Ginny L my indispensable nurse who works tirelessly to help our patients in every way possible and always with a smile and a chuckle
Rebecca my office manager of twenty five years who does all those behind the scenes things that make our office the best there is
Ginny C with the best phone manner on the planet
Regina our medical assistant who helps in so many ways
Our new addition nutritionist Rick who has taught us so much about the role of diet in treating and preventing illness
Our talented phlebotomist and Redskins Aficionado Chase
Cindy who keeps everything so well organized
Brendan and Erin the most wonderful son and daughter – in–law anyone could ask for
Daughter Michele my medical alter ego and newly board certified surgeon! Now working tirelessly mastering the trade of vascular surgery at Emory
To wife Nancy, the wind behind my sails
And of course you our wonderful patients
Have a Happy Holiday. We will see you back on Monday
 Almost all the publicity on the recent guidelines from the American Heart Association has centered on the use of statins. However a whole section was devoted to “Life Style Changes”. A group of experts reviewed the literature from 2001 onwards and concluded that aerobic physical activity such as brisk walking for 40 minutes at a time done 3 to 4 times per week will reduce blood pressure on average by 2 to 5 points systolic (the higher number) and 1 to 4 points diastolic (the lower number). Though that might not seem like a lot for many people it can be the difference between going on blood pressure medicines or having to increase the dose to get to goal.
Almost all the publicity on the recent guidelines from the American Heart Association has centered on the use of statins. However a whole section was devoted to “Life Style Changes”. A group of experts reviewed the literature from 2001 onwards and concluded that aerobic physical activity such as brisk walking for 40 minutes at a time done 3 to 4 times per week will reduce blood pressure on average by 2 to 5 points systolic (the higher number) and 1 to 4 points diastolic (the lower number). Though that might not seem like a lot for many people it can be the difference between going on blood pressure medicines or having to increase the dose to get to goal.
Similarly, moderate physical activity will lower LDL (lousy cholesterol) by 3-6 mg. More intensive physical activity results in further decreases. The effects on HDL or good cholesterol is less clear.
Importantly, dietary changes such as more fruits, vegetables, nuts, whole grains. and low fat products, in conjunction with exercise and weight loss, all help make for a healthier heart.
Not a patient yet but wish to get our weekly e-mail medical news summary and be able to ask questions of the doctor? Click Here
 “All good things must come to an end…” Well, hopefully not completely…
“All good things must come to an end…” Well, hopefully not completely…
While it is true that my 4-month fellowship in Tanzania “has come to an end” it is with the greatest of hope that the foundations in which accomplishments were achieved are sustainable and will continue to foster even greater successes in the months and years to come.
Supporting PSI the last few months has been one of the most life changing and rewarding experiences. PSI has established a new Health Services department that will focus primarily on supporting the franchise clinics with additional services to assist the people and communities of Tanzania. Health Services will work to educate, train, and develop providers in clinics to offer high quality health services; and will continue to work to insure those high quality standards are maintained.
Previously, PSI was supporting Family Planning services. During my tenure here, we have launched cervical cancer prevention and treatment programs, as well as programs for prevention of childhood illnesses. Near the end of my fellowship, PSI began launching a third additional service to provide safe Post Abortion Care. Implemented programs will heavily impact morbidity and mortality in women and in children under the age of five.
As I return home to the United States, I search my memories and experiences to define what the past four months have meant. All the superlatives come to mind “life changing”, “unbelievable”, “amazing”, “eye opening”, but what do those terms mean? For me, they serve as a springboard to advocate the need for improved health services in underdeveloped communities. To drive home this point, I go back to a heart wrenching fact I learned while I was here and I posted in an earlier blog. Tanzania is a country of 43 MILLION PEOPLE. It is twice the size of California, yet the country has ONE HOSPITAL that provides chemotherapy treatments… and this is merely just one example of the need to improve access to life saving medical care; unfortunately, there are so many more.
I want to thank Pfizer for the opportunity to become a part of the Global Health Fellows program. Without corporations who are truly dedicated to social responsibility, the path to identifying the tremendous need for support would be much more difficult to navigate. As Pfizer continues to develop medications and develop its people who can develop innovative strategies, there will be continued hope for UNDER developed nations.
Not a patient yet but wish to get our weekly e-mail medical news summary and be able to ask questions of the doctor? Click Here
 The new guidelines are a joint effort of the American Heart Association, the American College of Cardiology, and the National Heart, Lung, and Blood Institute to revamp guidelines on how to reduce heart disease and stroke risk. Though most of the press coverage has been about cholesterol guidelines it is important to emphasize that half the report was devoted to lifestyle modifications and the importance of us collectively and individually getting our weight down. The reports well document that our collective lack of physical activity, the kinds of foods we are eating, and the quantity of foods we are eating is greatly contributing to the epidemic of diabetes and vascular disease we are seeing as evidenced by heart attacks, sudden death, and stroke.
The new guidelines are a joint effort of the American Heart Association, the American College of Cardiology, and the National Heart, Lung, and Blood Institute to revamp guidelines on how to reduce heart disease and stroke risk. Though most of the press coverage has been about cholesterol guidelines it is important to emphasize that half the report was devoted to lifestyle modifications and the importance of us collectively and individually getting our weight down. The reports well document that our collective lack of physical activity, the kinds of foods we are eating, and the quantity of foods we are eating is greatly contributing to the epidemic of diabetes and vascular disease we are seeing as evidenced by heart attacks, sudden death, and stroke.
The reports solidify the safety and role of statins in reducing cardiovascular disease. The statin class of medications have been with us now for four decades and this report widens the audience of people who should consider them.
When patients have asked me over the years about the safety of statins I have half jokingly suggested that they should be in the drinking water. Though we are not yet to the point where anyone is advocating putting these medications in the drinking water – in some parts of the world there has been serious talk of giving everyone a “poly pill” of statin, aspirin, and blood pressure lowering medicine with the expectation that cardiovascular disease would dramatically drop.
In regards to cholesterol the report recommends that everyone with known heart disease and everyone with diabetes be on a statin, regardless of their cholesterol numbers. Furthermore, every one with an LDL “lousy” cholesterol of 190 or more be on a statin, and everyone at increased risk for heart disease consider being on a statin. How do you know if you are at increased risk? One way is to use the excel spread sheet calculator they have created and vetted http://static.heart.org/ahamah/risk/Omnibus_Risk_Estimator.xls
If your risk of having a heart attack, dropping dead, or having a stroke is greater than 7.5% over the next ten years it is recommended that you too be on a statin.
The panels of experts who wrote the reports tired to review and critique the world’s vast literature on these issues and to consolidate and come up with sensible recommendations. Their effort is admirable. It is by no means the last word and will be updated regularly. In future posts I will be exploring some of issues and controversies discussed in the reports including more about lifestyle and weight loss measures, concerns about statins causing diabetes, what to do about people who are intolerant of statins, management of elevated triglycerides, the role of heredity in heart disease, and how newer modalities such as the VAP profile may fit in.
Not a patient yet but wish to get our weekly e-mail medical news summary and be able to ask questions of the doctor? Click Here
 Trans fats are fats that get hydrogen atoms added to their structure (a carbon chain). Food chemists started ‘hydrogenating’ fats as a way of keeping vegetable oil-containing foods from going rancid. This was done for two reasons: because consumers basically don’t like chemical preservatives being added to their foods; and because the food companies were too cheap to use natural preservatives (like vitamin E or fat-soluble vitamin C). Food which contained these fats included crackers, cookies, chips, and other products that had to sit on shelves for a long time. The American food supply became, in effect, a ‘living laboratory’ to test the effects of these fats on a large population, long before these should have been tested for safety in humans.
Trans fats are fats that get hydrogen atoms added to their structure (a carbon chain). Food chemists started ‘hydrogenating’ fats as a way of keeping vegetable oil-containing foods from going rancid. This was done for two reasons: because consumers basically don’t like chemical preservatives being added to their foods; and because the food companies were too cheap to use natural preservatives (like vitamin E or fat-soluble vitamin C). Food which contained these fats included crackers, cookies, chips, and other products that had to sit on shelves for a long time. The American food supply became, in effect, a ‘living laboratory’ to test the effects of these fats on a large population, long before these should have been tested for safety in humans.
Hydrogenating fats makes them more saturated, which was one clue that they might not be so good for us. The second came from studies in mice, which found that trans fats messed with key processes involved in fat metabolism. Those of us who were reading these studies knew what was coming, but not when it would arrive. After studies in human populations found evidence of higher risks for heart disease, clinical studies in human volunteers followed. These found that trans fats raised our bad (LDL) cholesterol more than even saturated fats did. Even worse, while saturated fats raise both bad and good (HDL) cholesterol, trans fats lower HDL. The experiment is now over, and the score is still: Food companies 1, American consumers, zero.
Rick Weissinger, MS, RD, LDN, CPT
Author, WHAT THE EXPERTS SAY ABOUT FOOD AND CANCER
Co-author, NUTRITION GUIDE FOR CLINICIANS, editions 1 and 2
Web site: www.idomnt.com
 As part of our new cardiovascular risk assessment (the VAP test) we are analyzing not just the amount of LDL or “lousy” cholesterol in the blood but also the pattern of the LDL. Pattern “A” refers to large fluffy particles which are less damaging to blood vessels vs pattern “B” which refers to smaller and denser particles that tend to stick around longer and are more damaging to blood vessels. If you have a pattern “B” then you are twice as prone to have a heart attack or die suddenly from your heart disease. Heredity plays a role in which pattern you have but the good news is that lifestyle changes such as increased exercise and weight loss can help move those with pattern “B” to pattern “A” Simple changes in diet as advised by our nutritionist Rick, and certain medications can all play a beneficial role.
As part of our new cardiovascular risk assessment (the VAP test) we are analyzing not just the amount of LDL or “lousy” cholesterol in the blood but also the pattern of the LDL. Pattern “A” refers to large fluffy particles which are less damaging to blood vessels vs pattern “B” which refers to smaller and denser particles that tend to stick around longer and are more damaging to blood vessels. If you have a pattern “B” then you are twice as prone to have a heart attack or die suddenly from your heart disease. Heredity plays a role in which pattern you have but the good news is that lifestyle changes such as increased exercise and weight loss can help move those with pattern “B” to pattern “A” Simple changes in diet as advised by our nutritionist Rick, and certain medications can all play a beneficial role.
Not a patient yet but wish to get our weekly e-mail medical news summary and be able to ask questions of the doctor? Click Here
 We Have Answers To Your Health AND Wellness questions but we need questions to give answers to! Just go to olneymywellness.com/healthblog post your question, and the olneymywellness health care team will get right on it.
We Have Answers To Your Health AND Wellness questions but we need questions to give answers to! Just go to olneymywellness.com/healthblog post your question, and the olneymywellness health care team will get right on it.
As mentioned earlier we are using a new technology in our office to help better define who is at higher risk of developing clogged arteries and to help tailor the best therapies to prevent heart attack and stroke. Our new “toolbox” is the VAP profile and within that toolbox are a number of new tools in addition to the standard Total cholesterol, HDL (good), LDL (bad) and triglycerides. One of those tools is checking for something called Lipoprotein (a) or Lp(a) for short. Lp(a) is a cousin to a protein called plasminogen which helps break down blood clots. In people who have high levels of Lp(a) the plasminogen doesn’t work as well and hence they may be more prone to form dangerous clots. If you have a high Lp(a) level you may benefit from being on even more aggressive weight loss and exercise programs as well as appropriate medication to help lower risk. Lp(a) problems can run in families particularly those where heart attacks have occurred at an early age. Lp(a) levels generally should be less than 10 but tend to run higher in African Americans. We will discuss other tools in our new VAP toolbox in upcoming posts.
We are transitioning to a newer technology to check your cholesterol and risk of developing clogged arteries. This newer technology is known as the “VAP” profile and has the potential to give more useful information than the standard Total Cholesterol, HDL (Happy), LDL (Lousy), and Triglycerides. These more detailed reports may help us to further individualize your treatment and medications. We will explain these new reports in further blog posts and when you come in for your physical and visits to go over your lab results. Of course no medicine takes the place of exercising regularly and keeping your weight down to avoid diabetes. Many of our patients need help in getting their weight down which is why we have worked hard to develop our own Healthy Eating And Weight Loss Program.
 Yvette Is One Of Our Drug Reps Who Sends This Fascinating Post From Tanzania Where She Is Exploring the Culture & Medical Care
Yvette Is One Of Our Drug Reps Who Sends This Fascinating Post From Tanzania Where She Is Exploring the Culture & Medical Care
|
 Day 13 and fnally able to get online to find out what the new rates will be! Gone are the constant and ever changing error messages. Unfortunate that with two years for the State of Md and Federal gov to prepare it was such a mess at first.
Day 13 and fnally able to get online to find out what the new rates will be! Gone are the constant and ever changing error messages. Unfortunate that with two years for the State of Md and Federal gov to prepare it was such a mess at first.
One hope of the exchange was to lower rates by fostering competition among the insurance companies. However Aetna (profits of 1.66 Billion last year), and Cigna (1.62 Billion) have so far decided not to participate in the individual and family exchange for fear that their profits will be impacted leaving United, Carefirst, and Kaiser as the only major participants. No surprise then that the rates look similar to what was being offered previously.
Will enough healthy people join to pay for those with lots of medical expenses and, if not, who will pay the difference? Will Aetna, and Cigna continue to stay on the sidelines? Will United with profits last year of 7.2 billion dollars continue to participate if their profits go down? Stay tuned.
In most cases – 8 – 8 ounce glasses of water is sufficient for the day (64 ounces) – I am on a weight program and plateaued – it has been suggested that I drink 10 glasses per day – is this safe since I take diuretics?
As I get older, now 65, I find that excercise is causing me to get minor injuries. If it isn’t a sore back after yoga then it’s a sore achilles tendon after walking on the treadmill. Other than swimming, what excercises can you suggest that are suitable for a guy who thinks he’s in ok shape?
I am over 65 and have had my routine pneumonia shot. I heard there is there a new vaccine available for my age group. Do I need a booster?
 Food and Cancer” and “The Psychology of Weight Loss” talks about the role our diets play in influencing our risk of cancer and present evidence suggesting that modifying our diets may modify our risk.
Food and Cancer” and “The Psychology of Weight Loss” talks about the role our diets play in influencing our risk of cancer and present evidence suggesting that modifying our diets may modify our risk.
 Last year my husband and I were given the extra-strength flu shots intended for senior citizens. Are they available again this year? Did any studies show they were better than regular flu shots? We haven’t heard anything about them this year.
Last year my husband and I were given the extra-strength flu shots intended for senior citizens. Are they available again this year? Did any studies show they were better than regular flu shots? We haven’t heard anything about them this year.
(edited from the FDA website) The extra strength “Fluzone High-Dose” flu vaccine is again available and we have an ample supply in our office. This is the fourth flu season that it has been available. The vaccine is preservative free and is covered by Medicare. It is not a live vaccine and can be given to those with compromised immune systems.
The High-Dose vaccine has four times the amount of “antigen” in the hopes that it will be more effective in stimulating the immune systems of those 65 years and older who do not always get the full protection from standard flu shots due to our immune systems not being quite as robust as we get older.
The vaccine was initially tested in in 3,837 subjects 65 years of age and older. The initial study showed the vaccine to be safe without serious side effects. Those who received the higher dose produced more antibodies against the flu particularly the A strains and lesser so the B strain. As might be expected the greater amount of antigen caused more non serious side effects such as sore arm, headache and fever. The study was not designed to see if it actually prevented more flu cases. Based on the initial study the FDA approved the vaccine as an option for those over 65. The manufacturer agreed to collect data on 30,000 patients over 3 years to see if the vaccine was actually more effective than the standard flu shot in preventing the flu. An ongoing study designed to determine the effectiveness of the High-Dose vaccine in preventing illness from influenza compared to the regular strength is expected to be completed in 2014-2015.
The Bottom Line: The High-Dose flu vaccine is a reasonable option for those over 65. So far it appears promising and probably will be more effective in preventing the flu in those 65 and over though it may be another year or two before we can be more definitive.
Dr T
 I heard that we should be tested for hepatitis C. Does that mean everyone?
I heard that we should be tested for hepatitis C. Does that mean everyone?
(edited from the CDC) Hepatitis C virus (HCV) is an increasing cause of illness in the United States. Untreated over many decades approximately 5% of people with chronic hepatitis C will die of complications such as cirrhosis or liver cancer. Many persons with HCV infection do not recall or report having any specific risk factors such as injection-drug use, blood transfusion before July 1992 when a blood test was developed to protect the blood supply, having received chronic hemodialysis, being born to an HCV-infected mother, intranasal drug use, acquiring a tattoo in an unregulated establishment, being incarcerated, being stuck by a needle (e.g., in health care, emergency medical, home, or public safety settings) and multiple (>20) sexual partners.
At its peak in the 1960s there were a quarter of a million new cases per year in the United States. Presently there are less than 20 thousand new cases a year. The prevalence of HCV among persons born during 1945–1965 is 3.25% or five times higher than among adults born in other years. With the advent of new therapies that can eliminate hepatitis C the CDC has proposed one-time testing for persons born during 1945–1965.
The bottom line: if you have any of the risk factors listed above and have never been tested for hepatitis C you should consider a one time test. If you were born between 1945 and 1965 your chances of carrying hepatitis C are low but much higher than in more recent years and you also might consider a one time test. If you are a blood donor you do not need to be tested as you are tested each time you donate blood. We can include testing for hepatitis C with your routine physical blood work if you request it.
Dr T
 Looking to find a doctor’s office that practices medicine the way it used to be where people are friendly, efficient and get back to you with information, answers and treatment plans in a timely fashion?
Looking to find a doctor’s office that practices medicine the way it used to be where people are friendly, efficient and get back to you with information, answers and treatment plans in a timely fashion?[nivoslider id=”456″]
Click above to read the testimonials from our patients – your friends and neighbors who are already enjoying the benefits of the experienced care of Dr. Edward Taubman, the most pleasant office staff on the planet, and OlneyMyWellness – our homegrown and acclaimed wellness program. Click below to see how OlneyMyWellness can save you money while keeping you healthy and having some fun!
Dr. Taubman provided a careful and considered evaluation of the problem I presented and he offered an effective response. As always his highly professional approach was augmented by the sense of personal interest and care he projected.
Dr. Taubman, Nurse Ginny and the support team were cheery, helpful, competent and efficient. I was not rushed and was able to ask questions and receive thoughtful and understandable answers. I trust Dr. Taubman and am appreciative of the high quality of service that is rendered.
Thanks Dr. Taubman for catching it early on and saving my life. I don’t know how to thank you enough. Bob Y
Dr. Taubman is amazingly thorough. He listens and responds. The service he and his excellent and friendly office staff provide is top notch. We are lucky to have them as caring medical professionals. Nancy C.
Excellent consultation and establishment of health plan for 2013. Marilyn J.
I would never see any other GP. Jerry G.
He was great as always. Herbert P.
Dr. T is a good doctor, listens and always helpful. Paul P.
Great, very efficient. Answered all questions. Julien H.
I have only been going to Dr. Taubman’s office a few months, but I like him very much. I have difficulty finding a doctor in whom I can have complete confidence, but so far Dr. Taubman is one. He takes as much time as I need to get answers to my questions, which is not always the case with some doctors who seem to always be in a hurry. He is very calm, which instills confidence and, so far, has resolved my problems. Another important aspect is that his office staff is so pleasant and courteous that it makes clearing up medical problems a happier experience. John F.
Dr. Taubman is a very efficient and effective physician. He is very current, asks good questions (and is a good listener) and is technologically savvy. I always highly recommend him. Patricia R.
Dr. Taubman was professional, efficient and pleasant. The receptionist and nurse were as well. Thomas B.
I have a lot of confidence in his advice. Claire M.
Friendly staff and even though my husband did not schedule an appointment, the doctor asked him how he was doing and saw him after he was done with me. Catalina S.
Always helpful and informative. He clearly looks for my best interest. Paul P.
Knowledgeable and great for Recommendations. Thomas B.
Been seeing Dr. Taubman for over 20 years, always the finest care. Charles G.
Superior internist – pays close attention and gets deeply into the issues. Thorough and listened before offering comments – – eye contact and attention to my issues. His office staff is excellent. I could not ask for a finer physician – frankly it gets no better. Electronic scheduling was easy to use and worked perfectly. Arthur W.
Through, thoughtful, insightful, helpful. Fred B.
Always provides a very complete review of my illness. Ernesto A. G.
High quality professional services were provided as always. Joel C.
He listens first and then asks excellent questions. Walter H.
Dr. Taubman listens and responds to questions and is very personable. I was very happy with my visit. Frances R.
i always enjoy my visit with DR. T and love genny. love the whole staff. Glenna W.
My visit with Dr. Taubman was very good. He has an excellent. He was very thorough and I felt I had his undivided attention. Marilyn J.
As always Dr Taubman was kind, listened to me and offered good suggestions. Elizabeth D.
This was my 2nd visit and so far I am well pleased with Dr. Taubman’s professional manner and the way he addresses and evaluates my medical problems. I will highly recommend to friends and family. Joseph P.
Great! A good listener, good advice and has been a great doctor for years! Thank you, Dr. T. Barbara H.
Dr. Taubman is focused on the issues, answers all questions, provides a clear assessment and approach. Thomas B.
Only about 5 minute wait, which is great for a Dr. visit. New, positive vibe with the Wellness segment. I am confident in his knowledge and recommendations. Joseph F.
I really liked this doctor. He had a calm manner, was thorough, and explained things well. Betsy V.
Great doctor. Wonderful advice. I appreciated the time he spent with me. Never rushed. Lisa R.
This was a general physical. I like that Dr. T. listens, addresses concerns. He has helped me through the minor problems and a couple not-so-minor concerns in the 25 years he has been my primary doctor. Lucille M.
One of the very best. Michael G.
Dr. Taubman listens to your complaint and makes suggestions based on your responses. He is professional and has a good bedside manner. Mary R.
Dr. Taubman is my favorite doctor ever. Stephen L.
Dr. Taubman is the ultimate professional. He is thorough in his examination and makes one feel very comfortable. I’m happy to have him for my doctor. Dolores S.
Wonderful physician. Very comprehensive care. Mike B.
Efficient and thorough – I was not surprised that he adopted on-line scheduling, as he’s such a techie. Very little down time and everyone is so nice in that office. Even though I had not been there in years, Dr. Taubman and his staff remembered important details about me – unusual to find these days when the trend seems to be towards “fast food medicine.” Mary B.
Fantastic. Went in to seek relief from an arthritic condition. All med prescriptions were waiting for me at my local pharmacy immediately after the appointment. We developed several plans going forward to maintain a healthy lifestyle. Jared S.
Great service Vania B.
Ovarian cancer expert William P. McGuire III Medical Director of Inova  Health’s Gynecological Cancer Outreach Program discusses his experience treating ovarian cancer over the past 4 decades. Topics discussed include:
Health’s Gynecological Cancer Outreach Program discusses his experience treating ovarian cancer over the past 4 decades. Topics discussed include:
You can reach Dr. McGuire to schedule a consultation or second opinion at 703-970-6545 and ask for Rubi
3289 Woodburn Road Suite 320 Annandale, VA 22003 Like What You Are Seeing (and Hearing) Please Share This Post With Your Friends By Clicking On the Links Below Not Already Receiving Weekly E-mail summaries of Dr T”s Health Blog? Click Here To Register
OlneyMyWellness is pleased to have Rick Weissinger RD, MS, CPT join our wellness program. Rick is the author of a number of publications including nutritional handbooks for medical students, “The Psychology of Weight Loss”, and his newest book “What The Experts Say About Food and Cancer”. Rick uses the latest science on nutrition to help people lose weight and manage medical problems such as arthritis, diabetes, GI ailments, heart disease and who are interested in lowering their risk of cancer. Rick will be available in our office to see patients by appointment. For more information about our weight loss program click here or Call us at 301-774-5400 to make an appointment with Rick to help manage your medical problems through diet and to be placed on our waiting list for the next weight loss session.
 Are you at high risk for colon cancer?
Are you at high risk for colon cancer?  This podcast is for patients and families who would like to understand more about the known hereditary causes of colon cancer and the role of genetic counseling and testing. Topics covered include:
This podcast is for patients and families who would like to understand more about the known hereditary causes of colon cancer and the role of genetic counseling and testing. Topics covered include:
Dr. Taubman is a is a local expert on the hereditary aspects of cancer. He is a graduate of the City of Hope Program in Cancer Genetics and a member of the Fischer Center for Familial Cancer Research at Lombardi Cancer Center and sees patients in consultation who may be at high risk for hereditary cancers.
Questions, suggestions or comments about our podcasts? E-mail us at olneymywellness@olneymedical.com
roasted Brussels sprouts
Have a recipe you would like to submit? click here
 Are you at high risk for breast or ovarian cancer? This podcast is
Are you at high risk for breast or ovarian cancer? This podcast is  for patients and families who would like to understand more about the known hereditary causes of breast and ovarian cancer and the role of genetic counseling. Topics covered include:
for patients and families who would like to understand more about the known hereditary causes of breast and ovarian cancer and the role of genetic counseling. Topics covered include:
Dr. Taubman is a is a local expert on the hereditary aspects of cancer. He is a graduate of the City of Hope Program in Cancer Genetics and a member of the Fischer Center for Familial Cancer Research at Lombardi Cancer Center and sees patients in consultation who may be at high risk for hereditary cancers.
Questions, suggestions or comments about our podcasts? E-mail us at olneymywellness@olneymedical.com Confused as to what a Medical Power of Attorney otherwise known as an “Advance Directive” is and why you should have one? Well you have come to the right place. OlneyMyWellness affiliate Attorney Lynn Boynton explains it all.
Confused as to what a Medical Power of Attorney otherwise known as an “Advance Directive” is and why you should have one? Well you have come to the right place. OlneyMyWellness affiliate Attorney Lynn Boynton explains it all.  Topics covered include:
Topics covered include:
You can reach Lynn Boynton at 301-872-1696 or lcb@eqkmrh.com
33 Wood Lane Rockville, Maryland 20850OlneyMyWellness members receive a free consultation with Lynn and leave with a fully executed Medical Power of Attorney.
Questions, comments or suggestions about our podcasts? E-mail us at olneymywellness@olneymedical.com
Have a recipe you would like to submit? click here
Curves wants to incentivize you to start working out and stay fit!
OlneyMyWellness members will save 75% on joining and pay only $39 a month, a discount of $5 per month off the regular fitness membership rate for new members.
Call 301-260-7681 to make an appointment and learn more.
*Offer based on first visit enrollment, minimum 12mo c.d./e.f.t. program. Discount applies to initial service fee. Not valid with any other offer. Valid only at the Olney Curves location.
Take our diabetes quiz (modified from WebMD) and then hit Submit to see how you scored and to receive instructions on how to get your free tasty low calorie frozen yogurt treat (limit 1 per member)[WLQuiz_4 Diabetes Quiz Part 1]
Olney Medical was started by Dr. Taubman in 1979 and has since attended to tens of thousands of patients in the greater Olney area. The practice has repeatedly been rated by patients and physicians as “Top Doc” in Washingtonian and Checkbook Magazines. Dr. Taubman, in addition to his expertise as a primary care physician, is also a local expert in the hereditary aspects of cancer and is a graduate of the City of Hope Program in Cancer Genetics and is a member of the Fisher Center for Familial Cancer Research at Georgetown Lombardi.
For more information and about our practice including office and lab hours visit olneymedical.com
Famous icecream, bakery and cafe – serving muffins, bagels, espresso, donuts and cupcakes, open every day at 6 am. Present your OlneyMyWellness card and owner Tom Orban will give you a discount of 10%. OlneyMyWellness members
take our diabetes quiz and get a free Sprinkles sugar free (soft serve) frozen yogurt, at only 8 calories per fluid ounce called “Sprinkles 8”
 Dr. Taubman is a is a local expert on the hereditary aspects of cancer. He is a graduate of the City of Hope Program in Cancer Genetics and a member of the Fischer Center for Familial Cancer Research at Lombardi Cancer Center. He has given numerous lectures to physicians on how to screen for hereditary cancers and has written an article on the subject. Dr. Taubman sees patients in consultation who may be at high risk for hereditary cancers.
Dr. Taubman is a is a local expert on the hereditary aspects of cancer. He is a graduate of the City of Hope Program in Cancer Genetics and a member of the Fischer Center for Familial Cancer Research at Lombardi Cancer Center. He has given numerous lectures to physicians on how to screen for hereditary cancers and has written an article on the subject. Dr. Taubman sees patients in consultation who may be at high risk for hereditary cancers.
Visit their new fully equipped Official Spinning® Facility in Sandy Spring Maryland.
Offering personalized private cycle classes – when you want them – without a gym membership, contracts to sign or hidden fees.
OlneyMyWellnessMembers get 10% off spinning classes packages for and get a special 1 time 50% off Body Composition testing.
Contact owner Wendye Tobb for codes to use these discounts at their online store. Try a class – first class free!
 All Care helps patients receive quality care in the comfort of their own home and provides staffing for in home personal care, companionship, meal preparation, medication remindners, transportation & errands and light housekeeping.
All Care helps patients receive quality care in the comfort of their own home and provides staffing for in home personal care, companionship, meal preparation, medication remindners, transportation & errands and light housekeeping.
Show your OlneyMyWellness card and in addition to a free consultation and R.N. assessment (an $85 value) Owner Roger Zeender will give $100 off initial billing.
301-604-CARE
info@allcareassociates.com
Fitness studio has been in business for 7 years and has a loyal and growing clientele Enjoy this immaculately kept gym and no waiting to use the modern equipment.
OlneyMyWellness members present your membership card and owner John Torregrossa will waive the joining fee (a $150 savings) and reduce your monthly fee from $42 to $35 and throw in a free personal training session worth $100.
740 Cloverly Street
Silver Spring MD
call 301-384-0054 and ask for John to set up an appointment
You’ve worked out, watched your weight, seen your doctor. Now its time to have some fun. [nonmember]Members must be logged on to proceed.[/nonmember]
[ismember]Get Orioles Tickets Click Here![/ismember]
 I am a partner at the law firm of Ethridge, Quinn, Kemp, McAuliffe, Rowan & Hartinger. I specialize in estate planning, probate and residential and commercial real estate. We have offices in Frederick and Rockville.
I am a partner at the law firm of Ethridge, Quinn, Kemp, McAuliffe, Rowan & Hartinger. I specialize in estate planning, probate and residential and commercial real estate. We have offices in Frederick and Rockville.
As a benefit to OlneyMyWellness members I am pleased to offer a
30-45 minute free consultation which will include preparation of medical powers of attorney and advanced medical directive at our initial meeting. You will leave my office with completed, executed, notarized powers of attorney from our first meeting. I am happy to offer this free service as it pains me when a client becomes incompetent or gets sick and they didn’t have these important documents in place. They are forced to go through a guardianship proceeding which can cost thousands of dollars and takes many months. All of this can be avoided by having these documents prepared. If this saves one family from going through a guardianship proceeding, it is worth it.
Lynn Caudle Boynton
Ethridge, Quinn, Kemp, McAuliffe, Rowan & Hartinger
33 Wood Lane
Rockville, Maryland 20850
lcb@eqkmrh.com
www.eqkmrh.com
301-762-1696
301-762-7691 facsimile
Olde Key Title, LLC
33 Wood Lane
Rockville, Maryland 20850
lboynton@oldekeytitle.com
www.oldekeytitle.com
http://blog.oldekeytitle.com/
301-294-3333
Subscribe to Olde Key Title’s blog (http://blog.oldekeytitle.com/) and receive $100 off our settlement fee!*
*For Maryland cases only; not permitted in DC.
 Visit EYEWorks Vision Care Center in Olney Village Center and as a member you will receive:
Visit EYEWorks Vision Care Center in Olney Village Center and as a member you will receive:
-50% off eye exam
-50% off any frame in stock
-$50 off any contact lens packages
EYEWorksOlney
Present your OlneyMyWellness Membership card to Quality Optical – the optical store affiliated with Medical Eye Center with convenient locations in Olney and Columbia. OlneyMyWellness Members receive:
-$40 off on a new pair of eyeglasses
-Free MVA Screening Exam and form filled out by Medical Eye Center
 Harriet Breslow, L.C.S.W.-C HarrietBreslow.com
Harriet Breslow, L.C.S.W.-C HarrietBreslow.com
I Provide counseling to couples, families, individuals, and children. My belief is that most people already have the strength and resources to solve their own problems, and what I do best is help them tap into their own resources to find the answers they are seeking. Clients often believe that deep-seated problems require long-term therapy. They are always surprised that with my technique they can achieve the same effective results as with long-term therapy in a fraction of the time.
I have been in practice for over 37 years. I have seen the trauma caused to both couples and their children when divorce has been achieved by an angry litigation process. It is wonderful to know that there is now a respectful alternative to litigation, a collaborative divorce, which allows each person to maintain his or her own self-respect as well as give respect to the other party.
I am happy to give discounts of 20% to OlneyMyWellness members for services that are not covered by insurance such as parent coordinator, and collaborative divorce coach. A parent coordinator works with couples who need help with co-parenting after a divorce. A collaborative divorce coach is usually a mental health person trained in the collaborative techniques who works as a team with the lawyers representing each party.
Feel free to contact me by e-mail at harriet@breslow.org or phone 301-983-1321
OlneyMyWellness members receive 20% off on acupuncture and wellness services by licensed acupuncturist and wellness coach Trish Twiford MAC LAC
OlneyMyWellness members receive 20% off on yoga, kids yoga, acupuncture, massage, hoopfit, meditation, reiki and the newest fitness rage Zumba
Have those unsightly spider veins removed. 20% off * by our affiliate vascular vein specialists Horizon Vascular. Call 301-762-1560 to set up an appointment Horizon Vascular Specialists*
*due to Medicare regulations this discount is not available to Medicare enrollees
OlneyMyWellness members receive 20% off on teeth whitening by Dr. Stanley Cohen of Family Dentistry

Visit Stanley Cohen DDS
OlneyMyWellness members receive up to a 15% discount!*
visit skin matters
visit Dr. Len Hammer
*due to Medicare regulations this discount is not available to Medicare enrollees
Show your OlneyMyWellness card and receive 15% off brunch, lunch, or dinner (except Holidays)
The Inn at Brookeville Farms
19501 Georgia Avenue
Brookeville, MD 20833
Phone (301) 924-6500
For Additional Information Contact
info@brookevillefarms.com
Chef Tony’s Welcomes Olney MyWellness Members with a fantastic offer…
Flash your OlneyMyWellness card and receive 15% off all food items. In addition be on the lookout for specials exclusive to OlneyMyWellness members.
 From the Chefs site…
From the Chefs site…
Great food doesn’t have to be complicated or expensive.
I have made it a personal mission to work with local farmers, cheese producers, fish mongers and people who genuinely care about quality and great service. Creating a strong sense of community is an important philosophy at Chef Tony’s and we do as much as we can to support local businesses and philanthropic causes.
My menus are created daily to highlight our Mediterranean flare with the freshest produce and unique “catches of the day”.
Foods that are in season are naturally the most flavorful, fresh and simple to work with. You’ll have to either trust me or come test this theory for yourself.
Stop in and experience gourmet caliber cuisine at great prices… One visit and we’re confident that you’ll be back with your family and friends.
Eat Well. Be Well. Live Well.


al SOSPIRO Trattoria Romana & Wine Bar is now an affiliate of OlneyMyWellness!!
Chef Antonio Lombardi takes pride in cooking sumptuous foods that are simmered in healthy Mediterranean oils and food flavorings. Visit Chef Lombardi and flash your OlneyMyWellness card and receive 15% off all food items. In addition be on the lookout for monthly specials exclusive to OlneyMyWellness members.

18035 Georgia Avenue right in the heart of Olney
call 301-570-3185 to make a reservation
Synergy members love their fitness center with all sorts of extras like yoga and Zumba. For OlneyMyWellness members they will waive the joining cost and lower the going rate by $10 per month. Call 410-964-9858 to make an appointment and learn more.
 This first class fitness center is known for excellent staff, state of the art facilities and personalized attention that is second to none.
This first class fitness center is known for excellent staff, state of the art facilities and personalized attention that is second to none.
OlneyMyWellness members receive a two week free trial including a free session with a personal trainer ($120 value), no joining fees (save $99), a half hour massage with a nationally certified Massage Therapist ($50 value), and an amazing rate of just $30 per month instead of the usual $47.50
Visit them at above the IceHouse in Laurel. http://www.wellnessforlifefitnesscenter.com/
 This club has it all including pool, racquetball, basketball, pilates, zumba, indoor golf, kick boxing and just about anything else you can think of. Give them a try – OlneyMyWellness members have no joining fee at any Sport&Health Club including Rio, Lakeforest, and Bethesda. OlneyMyWellness members also get a free two week trial – Join now and get the first month free.
This club has it all including pool, racquetball, basketball, pilates, zumba, indoor golf, kick boxing and just about anything else you can think of. Give them a try – OlneyMyWellness members have no joining fee at any Sport&Health Club including Rio, Lakeforest, and Bethesda. OlneyMyWellness members also get a free two week trial – Join now and get the first month free.
Seneca Physical Therapy, long known for their expertise in rehabilitating injured elite and recreational athletes, developed Senecca Wellness and Fitness Center over 10 years ago and opened it to their patients and the general public.
Seneca Wellness and Fitness Center merges the world of fitness with the science of physical therapy, making exercise safer and more effective for their clients.
Your individual program is designed under the guidance and input of an exercise physiologist in a clinical environment. The individualized program is closely monitored, reviewed, and revised to meet your increased level of fitness.
Exclusive to members of OlneyMyWellness they will discount their current monthly membership fee by $7 per month and waive the joining fee.
Call them at 240-361-0668 and ask to speak with Robert or visit them at their website at Seneca Wellness & Fitness
OlneyMyWellness Members have the joining fee waived (a $125 value) and receive $7 off the going rate.
Join this fitness center www.americanfitnessexpress.com and have 24/7 access to work out! OlneyMyWellness Members pay only $15 per month and no joining fee. Speak to Owner Dan Surbrook at 410-489-9556 to arrange a visit.
3881 Ten Oaks Road #B Glenelg, MD 21737
World Class Fitness Center with latest equipment, year round olympic sized pool, racquetball, tennis courts, and more. Aspen Hill Club will offer their lowest corporate rate, and in addition will waive the usual joining fee (a $175 value). Call 301-598-5200 to make an appointment and learn more.