If you are confused as to what your target blood pressure should be, you are in good company. Every decade or so the NIH/National Heart, Lung, and Blood Institute (NHLBI) convenes a group of experts to reach a consensus on the desired numbers. The most current national guidelines, known as JNC 8 (Eighth Joint National Committee), were released just last year and recommended a number of changes in target blood pressure recommendations for the systolic (the upper number) and the diastolic (the lower number).
- For most people the goal remained to get the blood pressure below 140/90
- However, for those over the age of 60 the goal shifted upwards to 150/90
- For those with diabetes and kidney disease, the goal blood pressure was no longer a lower 130/90 but shifted upwards to that of the general population, (ie. 140/90 and 150/90 for those over 60). quality published (and peer reviewed) studies are in – expers out.
Why the upward change? Part of the answer lies in the changing role of the expert committee. In prior years the experts would pool their personal and research expertise, debate the meaning of the vast literature, iron out their differences, and come up with an updated set of recommended standards.
However, reflecting a pervasive trend in medicine nowadays called “Evidence Based Medicine,” the experience of experts (as well as your doctor) is increasingly minimized. In the Evidence Based Medicine era published studies are king. If they don’t support a point of view beyond a shadow of a doubt, then that point of view is not considered.
In this instance, since the literature to date has not conclusively shown that lower blood pressure is necessarily better and the opinions of the experts were throttled, the committee really had no choice but to set the target goals higher.
So, with that in mind, even though many physicians were uncomfortable with the recommendations, it seemed as if these were to be the new standard for probably another decade until JNC 9 would come along.
A New Standard? – Treat by press release
Last month the NHLBI issued a press release. It said that an ongoing trial that they were conducting known as SPRINT that began in 2013 and which was scheduled for completion in 2018 was stopped early because it showed that treating the upper level of blood pressure (systolic) to a target of 120 seemed better than treating to a less stringent goal of 140. This self-proclaimed breakthrough was quickly picked up by the news media; suddenly it seemed we needed to change our approach to hypertension and once again lower our target goals.
What wasn’t mentioned in the 30-second news flashes was that to get to a systolic blood pressure of 120 would often take up to four medicines, that only 9000 people were in the study, that diabetics were not part of the study, and that the study was yet to be published – let alone reviewed by outsiders; which is an important tenant of evidence based medicine.
Personally I think it was unfortunate that the NHLBI issued a press release on this. The media and the public do not understand that press releases are not the final word. It would have been better for the study to have been published first and critically reviewed by outside experts. For all we know outside experts might ultimately conclude that the study was flawed or stopped too early. So now what should patients and doctors do?
I do suspect that ultimately this newer study, once validated, will again tilt us towards tighter blood pressure goals. However, we have to recognize that medicine is not black and white; there are lots of grays. Arteriosclerosis and its complications are a lifetime in the making, perhaps even starting in the womb; and we may never have definitive answers from short term studies. Treatment decisions about blood pressure need to be individualized as much as possible. For the elderly, in particular, side effects secondary to excessive treatment causing falls, may be their biggest threat.
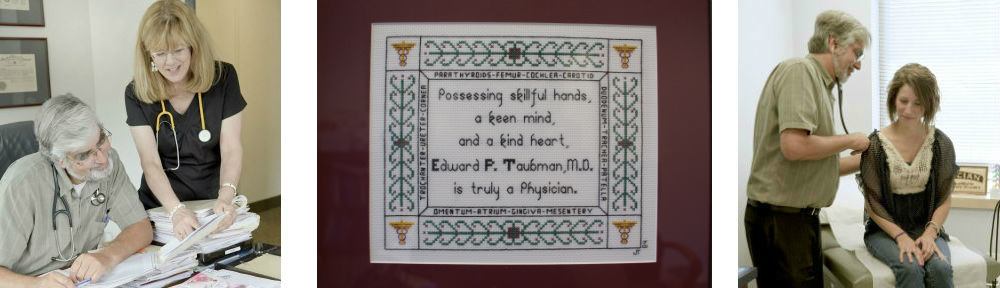
At the end of the day, guidelines should be recognized for what they are – guidelines. If your health care provider is deciding how to treat you strictly based on the guidelines on their iphone, it might be time to change. A nuanced and individualized discussion with an experienced physician who understands your needs should be your expectation.
Next Post: Cholesterol – How Low Should We Go?
This article first appeared in the November 11 2015 issue of The Greater Olney News