We now think of cancer as a disease of our genes – an accumulation of genetic mutations that may one day show up as a cancerous lump.
Genes are the instruction sets of life; we each start out with over 20,000 pairs of them in each and every one of our cells. As we grow and age, our cells are duplicated hundreds of millions of times, and with each cell division the genetic instruction set is duplicated, as well. Think of asking your secretary to copy by hand 20,000 books containing three billion letters, a hundred million times, and tell her or him that their job is dependent on no mistakes being made.
Part of the miracle of life is that we have evolved an elaborate set of genetic spell checkers that seek out and find genetic misspellings that may develop and fix them. Unfortunately, the system is not perfect; and genetic misspellings in a breast cell, say, can begin accumulating until a cancer develops. Many other factors are being increasingly recognized in the development of cancer, including environmental exposures that increase genetic damage and the role of our immune systems, which can seek out and destroy developing cancers. And there may well be a strong element of randomness, which some prominent researchers refer to simply as “bad luck. Nonetheless, around 5 percent to 10 percent of breast cancers have a strong hereditary component that can be passed on from one generation to the next. In some of these families, the cause has been linked to the genetic spell checkers themselves having genetic misspellings that have been passed down from generation to generation by both men and women over thousands of years. When these “guardians of the genome” are themselves defective, then lifetime cancer risk can rise dramatically. In the mid-1990s researchers separately discovered two different genes that, when misspelled, greatly increased a woman’s risk of developing breast cancer. The first discovered breast cancer-associated gene we now call BRCA1; the second discovered gene is BRCA2.
Recently, genetic testing companies have put together panels of many additional genes to test for breast cancer risk. These panels can sometimes add more confusion than clarity as they often find variations in genetic spelling of unknown significance in lesser-known genes.
Though most patients and physicians think of breast cancer when they hear BRCA, it is the ovarian cancer risk that is potentially more deadly. A woman who has inherited a deleterious BRCA gene has up to a 40 percent lifetime risk of developing ovarian cancer, compared to about a 1 percent to 2 percent risk in the general population.
Unlike breast cancer, ovarian cancer is not detected by self-exam, and screening tests have been repeatedly found to be ineffective. Thus, if a woman is found to have a pathogenic BRCA misspelling, otherwise known as a deleterious mutation, then her ovaries should be removed as soon as child-bearing is completed. Because of the high rate of breast cancer, some women elect to have bilateral mastectomies with reconstruction, while others choose intensive surveillance with MRI screening as a complement to mammography.
The incidence of these cancer-predisposing BRCA genes in the general population is about one in 400 to one in 1,000, with the incidence in the American Jewish population much higher at about one in 40. Given the high incidence in the Jewish population, a strong case can be made to offer BRCA genetic screening to all of Jewish descent. Ovarian cancer at any age, early breast cancer, bilateral breast cancer and male breast cancer should raise hereditary suspicions. If you come from a small family with mostly men, your cancer family history may not be a reliable indicator of your true risk. Before testing, patients should be counseled about the true meaning of not only positive and negative tests but also variants of unknown significance. Also, care needs to be taken to make sure the most appropriate person in the family, the one most likely to be positive, is tested first. A negative test in an individual only has true meaning when there is an identified deleterious mutation in the family.
When someone is battling cancer, hereditary counseling and testing often need to take a back seat. Unfortunately, when the crisis has passed, even at the best cancer centers, we may collectively forget to ask the question as to why the patient got cancer in the first place. Finding a culprit genetic misspelling in a cancer-prone family gives other family members a chance and a choice to be tested to see if they, too, are at very high cancer risk and to take preventative measures. Unfortunately, a recent study showed that only 3 percent of individuals at high risk of an inherited cancer syndrome ever get referred for cancer genetic counseling.
At the end of the day, we can’t do anything about “bad luck,” but we do have control of environmental exposures. Numerous studies have linked being overweight, hormone ingestion and alcohol consumption, even in small doses, to increased breast cancer risk. So if you are worried about breast cancer, try to eat less meat, consume more fruits and vegetables, minimize your alcohol consumption, start exercising and begin shedding pounds. If you family history is of concern, ask your doctor to refer you to a cancer genetic specialist.
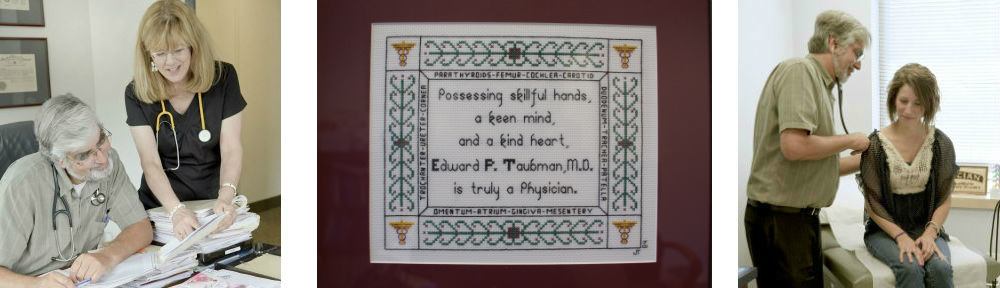
Dr. Edward Taubman has been practicing primary care medicine in Olney since 1979. He is a graduate of the City of Hope Intensive Cancer Genetics Program and a member of the National Society of Genetic Counselors andthe Fisher Center for Hereditary Cancer and Clinical Genomics Research.
This article first appeared in the Greater Olney News on October 28, 2015