The recent case of a Liberian with Ebola virus not being recognized by a Dallas emergency room provides a reason for me to get on my soap box and complain about the transformation of American medicine into a checklist mentality. While I understand that checklists can play important roles in certain industries – the classic case being pilots making sure flaps are up before takeoff and nurses in operating rooms making sure all instruments are accounted for after surgery – a checklist mentality has now permeated all aspects of medicine. The problem is there are now so many checklists to be completed that health care workers are too close to the checklist trees; and sometimes miss the big picture. Once checklist A has been completed, then it’s on to checklist B and so it goes, on and on – all in the name of good care. The problem is that medicine has a lot of subtleties; it’s not just black and white but lots of greys. Good clinical judgment cannot be captured by a checklist and good medical care requires great communication. This means people need to talk to each other – which is difficult when one is glued to a computer filling out checklists. Medicine is an art as much as a science; that’s why to become a doctor takes over a decade. There aren’t enough checklists in the world to ensure good medical care.
The recent case of a Liberian with Ebola virus not being recognized by a Dallas emergency room provides a reason for me to get on my soap box and complain about the transformation of American medicine into a checklist mentality. While I understand that checklists can play important roles in certain industries – the classic case being pilots making sure flaps are up before takeoff and nurses in operating rooms making sure all instruments are accounted for after surgery – a checklist mentality has now permeated all aspects of medicine. The problem is there are now so many checklists to be completed that health care workers are too close to the checklist trees; and sometimes miss the big picture. Once checklist A has been completed, then it’s on to checklist B and so it goes, on and on – all in the name of good care. The problem is that medicine has a lot of subtleties; it’s not just black and white but lots of greys. Good clinical judgment cannot be captured by a checklist and good medical care requires great communication. This means people need to talk to each other – which is difficult when one is glued to a computer filling out checklists. Medicine is an art as much as a science; that’s why to become a doctor takes over a decade. There aren’t enough checklists in the world to ensure good medical care.
Checklists in medicine evolved initially to keep insurance companies from denying payments for alleged lack of documentation and to help fend off lawsuits. The problem with checklists is that they are often used as excuses to allow less expensive (and less trained) personnel to provide care. Moreover, the checklist recepients have become immune to paying attention to the lists due to checklist information overload. And it’s not just checklists – All day long our fax machine and computer are spitting out voluminous computer-generated notes from doctors’ offices describing five minute visits for minor medical problems.
What we need in medicine is less time checking lists and more time for more qualified people to think and analyze. People need to get up out of their seats and away from their computers and to communicate the old-fashioned way – by talking.
In Dallas the hospital initially acknowledged that a nurse took a travel history and filled out a checklist, but the information never made it to those responsible for the care of the patient. Their most recent explanation as reported on CNN is “As a standard part of the nursing process, the patient’s travel history was documented and available to the full care team in the electronic health record, including within the physician’s workflow,” In other words blame now is being shifted from the nurse (her job ended when she put the travel checklist into the computer) to the “full care team”. Using the term “full care team” might be an artful way of saying the patient wasn’t actually seen by a doctor, but rather by a nurse practitioner or physician assistant.
Regardless of who saw the patient it is tempting to try to put the blame on the nurse, or the doctors, or conclude that their computer system just needs an upgrade to better flag alarming issues. The real problem is the electronic checklist mentality which is overtaking medicine. And though the bean counters would like us to believe that good medicine can be quantified and accomplished by more and more computerization, this should serve as a wake-up call to the contrary.
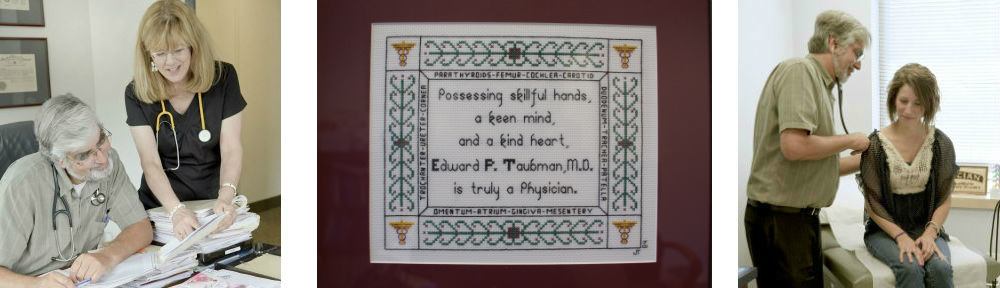
Until next week this is Dr. Ed Taubman primary care Olney MD 301-774-5400 where friendly and helpful people are ready to serve you and the doctor hasn’t forgotten how to pick up the phone to coordinate your care with your other health care providers.