This week, rather than delving in depth on a specific topic I thought I would get off my soapbox and summarize some recent literature that is of interest to me as a physician and which may perhaps have impact on health care in the not too distant future. Let me know what you think of this format!
This week, rather than delving in depth on a specific topic I thought I would get off my soapbox and summarize some recent literature that is of interest to me as a physician and which may perhaps have impact on health care in the not too distant future. Let me know what you think of this format!
-A number of articles and an editorial in the New England Journal of Medicine document that even though the media is focused on new and experimental treatments for Ebola that many lives can, and are being saved, with the use of intravenous fluids, attention to oxygen needs, and treatment of secondary infections. Though such treatments are commonplace in intensive care units such as those in our own community, they are lacking in Africa – which contributes to the high death rate there. In essence Ebola is a serious viral infection which can be treated with existing known management strategies.
-Previously I have touched on the childhood obesity epidemic. So how do we get adolescents, for instance, to cut back on the sodas they are drinking? In a study done by the Johns Hopkins Bloomberg School of Public Health adolescents going to the store were shown how many calories were in the beverages they were consuming vs how many miles they would have to walk to work off a single soda. The authors reported that “adolescents who were given caloric information associated with a sugar-sweetened beverage in a format they could relate to” ie how many miles they would have to walk to work off a single soda were more likely to purchase a smaller sized soft drink, choose a diet beverage, or forgo the beverage altogether. Makes sense to me. Seriously, maybe we should do the same thing on food labels in general.
-So, you’re a drug company and want to test to see if your new drug is better than a placebo (dummy or sugar pill). To get FDA approval you need to spend tens or even hundreds millions of dollars doing trials to prove your drugs are safe and effective. Sounds straight forward; but in actuality many people in drug trials are just like everyday patients – they often don’t take their medicines as directed – which means the researchers doing the study may get ambiguous results or need to enroll many more patients to find true differences among different treatments; doing so makes the trials that much expensive to do which ultimately drives up the cost of the new medicines.
As reported in Science some strategies being discussed to deal with this include putting microchips on pill bottles to show how often the bottles have been opened and even inserting microchips into the pills themselves that can radio to monitoring devices that they have actually been ingested! And finally, researchers have discovered what may be genetic traits that make some people inherently more predisposed to respond to dummy pills or just want to please; in drug trials they may be more prone to report benefits and not report adverse effects. If too many of those people are in drug trials they could influence the results in a way that makes it hard to tell if a drug was better than a dummy pill; in the future genetically testing for such traits to limit the number of such people in drug studies might one day increase the reliability of drug studies, reduce the number needed to find a benefit, and ultimately reduce the cost of bringing new treatments to market.
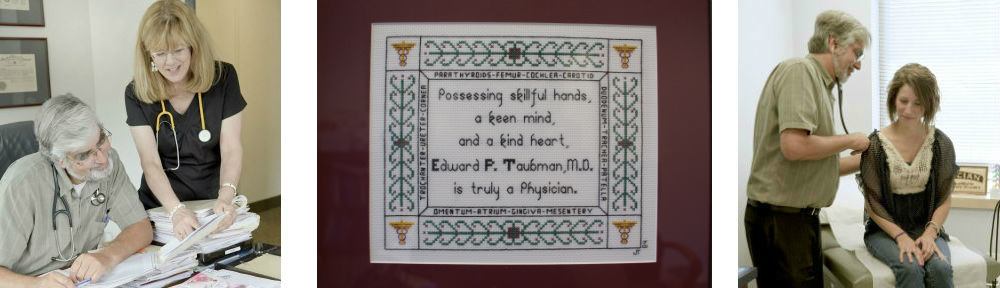
Until next week. Dr Ed Taubman, Primary Care, Olney MD 301-774-5400
Like what you are reading? Please share with others!