For most women routine pelvic examinations by their internist, family doctor, or gynecologist have become annual rituals. However, some recent recommendations have raised questions about the value of these exams and in the process confused many patients and physicians alike. Much of the confusion has to do with the terms “Well Woman Exam, PAP test, and “pelvic examination”. For most women these terms are synonymous. However, in the medical field they can be three separate things.
For most women routine pelvic examinations by their internist, family doctor, or gynecologist have become annual rituals. However, some recent recommendations have raised questions about the value of these exams and in the process confused many patients and physicians alike. Much of the confusion has to do with the terms “Well Woman Exam, PAP test, and “pelvic examination”. For most women these terms are synonymous. However, in the medical field they can be three separate things.
A PAP test, for instance, is a swab taken from the entrance to the uterus or womb. The purpose of the PAP test is to check for either early changes that could lead to cervical cancer, or the detection of the Human Papillomatous Virus (HPV) that causes the vast majority of cervical cancer. A PAP test requires a woman to be on an exam table, legs up in stirrups, with the insertion of a device known as a speculum which opens the vagina so that the cervix can be seen and the PAP smear of the cervix done.
A “Pelvic Exam” (sometimes called an “Internal”) starts out also with a woman up in stirrups. However, instead of inserting a speculum to visualize the cervix, this procedure involves the insertion of one gloved hand in the vagina and the other on the abdomen to feel if anything in between seems abnormally enlarged such as the uterus or ovaries.
A “Well Woman Exam” literally means an otherwise well woman visiting the doctor, discussing important issues such as heart health, diabetic tendency, osteoporosis screening, blood pressure checking, having a breast exam, and otherwise being appropriately examined which may or may not include a PAP smear being obtained or a pelvic exam.
The recent brouhaha which has caused all the confusion is really only about the value of that second element – the “Pelvic Exam” in otherwise healthy, non pregnant, asymptomatic women. Turns out that poking around with one hand in the vagina and the other on the abdomen rarely finds anything serious and occasionally results in surgery that in retrospect might not have been necessary.
That’s not to say that a pelvic exam couldn’t disclose factors of interest or importance to the patient or doctor such as the presence of non – cancerous “fibroids” or bladder “prolapse” – which might contribute to incontinence. Trying to catch early ovarian cancer is often cited as a reason to do routine pelvic exams. Unfortunately, repeated studies have shown that ovarian cancer is rarely detected on routine pelvic examination; for that matter there does not exist any reliable test for detecting early ovarian cancer in women who have no symptoms.
So, what does this mean for the average woman? The most important thing to understand is that women who are feeling well should still see the doctor from time to time to check their blood pressure, cholesterol, breasts, skin, and thyroid; and have referrals for preventative health measures as may be appropriate based on their family history and age, such as mammograms, bone density tests, and colonoscopies.
Women, between the ages of 21 and 65 still should have periodic PAP tests which still involves getting up on the exam table with legs up in stirrups. Current guidelines for women without symptoms and previously normal PAP tests support PAP testing every three years – though as newer technology to test for HPV is introduced, the recommended frequency for some women may decline.
So, in summary, should women give up going to the doctor for a well woman exam? Absolutely not.
Should women younger than 65 give up on PAP smears? Absolutely not.
Should all women regardless of age have an annual pelvic exam/”Internal”?? Not necessarily. However, keep in mind that part of the debate in medical circles revolves around the question as to how often doing the exam results in finding something significant in people who otherwise feel well. Part of the debate also revolves around cost effectiveness. The same argument could be made for not listening to people’s hearts with a stethoscope, or not listening to their lungs as that might result in further testing such as echocardiograms, chest xrays or CT scans without proof that doing so results in longer lives.
Importantly, none of this applies to women who have symptoms that could be warning signs such as abnormal bleeding, unexplained bloating or pains. If these persist, they require a complete exam regardless of age.
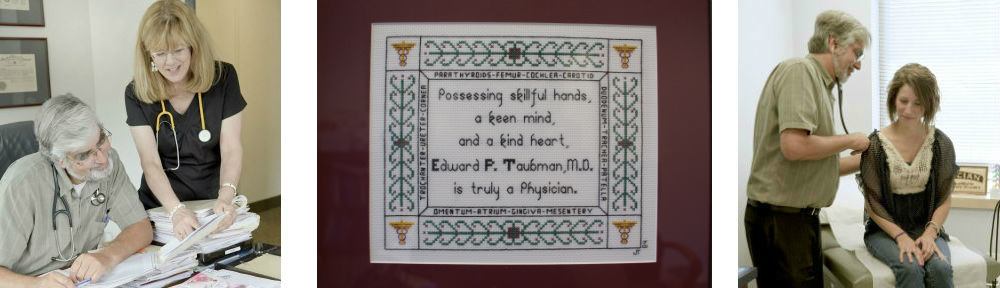
by Dr Ed Taubman Primary Care Physician Olney MD 301-774-5400
Once Again Voted Top Doctor “Washingtonian Magazine”
To Join my Health Blog and start receiving weekly e-mails of new informative posts click here
Follow me on fB facebook/olneymywellness